How to Prepare for an Insurance Treatment Review
As a behavioral health professional, you want to provide the best care for your clients and not have to limit their care due to insurance issues. It's understandable if you feel overwhelmed by the pending review, but there are ways to take charge of the situation. If you know how to prepare for a treatment review, you'll be ready to defend your client's care so you can continue treatment as planned — with peace of mind.
Table of Contents
What is an Insurance Treatment Review?
A treatment review also referred to as a utilization review, is when an insurance company contacts a therapist or other behavioral health care provider to ask them questions about the treatment of a client. The reviewer’s goal is to determine whether or not the treatment is medically necessary and part of an acceptable and effective treatment plan. The insurer will then decide if they will continue reimbursing for the behavioral health services under review. In most cases, especially for mental health services, the review is a standard expectation. It is routinely scheduled to happen on certain days/times (if telephonic). It is due by certain dates (if electronic) within that specific course of treatment, and this has been arranged by the staff member (telephonic/electronic) making the initial contact to state the person is there for services and the reason they need to be there. Unless records are requested for an audit, the treatment review will not be a surprise to the treatment facility.
Frequently Asked Questions About Mental Health Treatment Reviews
Treatment reviews can seem daunting if you don’t know what to expect or how to prepare. Let’s look at common questions regarding insurance reviews and different types of plans, so you’ll be better prepared to speak the language of insurers.
1. Who Determines Medical Necessity?
Although federal and state governments create some guidelines that health insurance companies must follow, it’s otherwise up to the insurer to decide what’s considered a medical necessity. If an insurance company decides a service is not medically necessary, they can deny a claim.

2. What Is Used to Determine Medical Necessity?
Medical necessity criteria vary between policies. However, some services are typically deemed medically necessary or unnecessary. For example, Medicare defines medically necessary as services or supplies needed to diagnose or treat a condition that meets “accepted standards of medicine.” However, Medicare does not cover medically unnecessary services such as:
- Evaluation and management services exceeding those considered medically necessary
- Excessive therapy or diagnostic procedures
- Exams, screening tests and therapies that do not relate to a client’s symptoms
Imagine a scenario in which you increase therapy sessions from once a week to three times a week for a client experiencing a crisis. Their Medicare plan may question whether or not these sessions are medically necessary or excessive.
Private insurers can set their own criteria as long they comply with state and federal healthcare laws. For example, Aetna lists the following criteria for medical necessity for health maintenance organization (HMO) plans:
- The service follows generally accepted standards of medical practice.
- The service is clinically appropriate in terms of type, frequency, extent and duration.
- The service is not primarily for the convenience of the patient or provider.
- The service is not more costly than an alternative service.
In other words, a client cannot solely desire treatment – it must be necessary for their medical health. Therefore, therapy must not only focus on personal growth and improving specific life skills, but also on relieving medical symptoms such as depression or anxiety. Typically, insurers will only cover the treatment of a diagnosis found in the Diagnostic and Statistical Manual (DSM). Lastly, a therapist cannot use any type of therapy they wish to treat a client. The reviewer must believe that the treatment is proven to be effective, and it must be the most cost-effective option.
3. How Is a Review Different From a Record Request?
Your practice may receive letters from insurance companies requesting patient records. They may call the record request a risk adjustment audit or data collection. The Centers for Medicare and Medicaid Services (CMS) uses risk adjustment audits to determine appropriate premiums. Generally, the goal of a record request is to find out the health status of beneficiaries so insurers can determine where to transfer funds. A record request is not about determining medical necessity or reviewing treatment plans. In the event of a record request, you can call the insurer and ask exactly what they need for the data collection and check state laws about releasing records. There’s no need to release your private psychotherapy notes.
4. How Is a Review Different From an Audit?
While a treatment review focuses on the necessity and effectiveness of your client’s treatment plan, an audit usually reviews documentation to confirm you’re following insurance plan documentation requirements. Insurance companies often randomly select care providers to review charts and other forms of documentation. An audit has nothing to do with reviewing the effectiveness of your treatment. You can obtain a list of documentation requirements for any insurance plan you provide to always be prepared for a random audit.
5. What Is a Clearinghouse in Healthcare?
Simply said, a healthcare clearinghouse plays the middleman between your practice and an insurer. When you’re ready to submit a claim for reimbursement, you can submit the claim to a clearinghouse rather than directly to the insurer. The clearinghouse will check for errors to help make sure your claim is accepted. Working with a clearinghouse can improve efficiency and simplify the billing process.
6. Fee-for-Service Contract vs. Capitation: What’s the Difference?
A fee-for-service (FFS) plan is a traditional insurance plan in which the insurer will either pay a physician or other health care provider directly or reimburse a client after they file a claim. Capitation, on the other hand, involves fixed monthly payments agreed upon in a contract between a care provider and an insurance company. With a capitation contract, a physician receives agreed-upon payments per patient enrolled in the health plan. The payments are decided a year in advance and remain the same throughout the entire year, no matter how often the patient needs services. Capitation helps health insurance companies control costs by discouraging physicians from providing more care than necessary. The main benefit for physicians is less bookkeeping and not needing to wait for reimbursement.
7. Fee-for-Service vs. Value-Based: What’s the Difference?
Value-based health care is when physicians are paid based on patient outcomes. Therefore, providers are rewarded for helping patients live healthier, happier lives. Value-based care differs from both capitation and FFS approaches because it focuses more on quality of care rather than quantity. This type of model is designed to provide lower costs and better outcomes for patients, higher patient satisfaction for providers and a healthier population with fewer claims.
Preparing for a Treatment Review
The best way to ensure a relaxed and effective treatment review is to prepare. We’ll show you how to prepare so you can approach an insurance review with confidence.
Why Is it Necessary to Prepare for a Treatment Review?
It’s best to carefully prepare for a treatment review so that you’re ready to fight for your client’s care and can respond confidently to any questions the reviewer may ask. If you don’t prepare for the review, you may not mention key information that could prove your treatment is medically necessary.
Tips for Preparing for a Treatment Review
The review itself may either be a phone conversation with an insurance plan or involve filling out a form electronically. Either way, you have a right to know exactly what to expect during a review. There’s no need for you to head into a review blindly. Here are ways to prepare:
- Call the insurer: The first step in preparing for a treatment review is to call the insurer and ask to schedule the review, allowing yourself enough time to prepare. Ask them what questions they’ll ask you during the review and find out what their medical necessity criteria entails. Unless records are requested for a random audit, the review is never a surprise call or notice by the insurance company. In fact, the person completing the insurance reviews for the practice or treatment facility typically schedules at least one concurrent review date from the initial admission review that has taken place. For the initial reviews, it is the facility/practice that contacts the insurance company, not the other way around. Most of the time, the insurance company will not even know someone is actively being treated until that facility communicates upon the patient’s entry, for need of billing.
- Interview the client: Interview the client whose treatment will be in review. Ask the client questions about their current symptoms, how the symptoms affect their life, and what they hope to achieve in therapy – all while keeping medical necessity criteria in mind.
- Coordinate care: Coordinate care with the client’s physicians and other therapists before the review, because you may be asked if you’ve done so by the reviewer. Electronic health record (EHR) software like ICANotes makes it easy to share information with other approved healthcare providers and coordinate care. For example, ICANotes connect with health information exchanges so you can securely access and share patient medical information electronically.

- Take better notes: Taking detailed notes during therapy sessions will help you with the review. Make sure to focus on listing symptoms that impair areas in your client’s life, such as insomnia or lack of appetite. Keep in mind that the reviewer will want evidence that a DSM diagnosis is present or suspected.
- Remember who you’ll be speaking with: Also keep in mind that you will be discussing a client’s treatment with a reviewer. Therefore, prepare to speak strictly about symptoms and proven treatments for the client’s diagnosis to prove medical necessity.
- Focus on your treatment plan: A critical aspect of your treatment review will be your treatment plan. A treatment plan is a tool used to effectively treat patients. It’s an organized detailed plan tailored to meet a patient’s need. It usually follows a simple format and often includes the patient’s diagnosis, treatment goals that focus on reducing specific symptoms, measurable objectives, interventions and a timeline for treatment progress. In other words, a well-constructed treatment plan will include all of the elements a reviewer will ask about. An easy-to-use EHR template can ensure you cover all the bases quickly and efficiently.
Learn More About Writing Individualized Treatment Plans
After you prepare for a treatment review, you’ll be ready to direct its course. It’s most important to have a detailed treatment plan in front of you during the review, so you’re ready to explain how you and your client meet the insurer’s medical necessity requirements. Here are tips for treatment review success:
- Discuss their diagnoses and medications: Know your client’s diagnosis and any comorbid diagnoses and how therapy reduces related medical symptoms. Also mention current psychiatric medications, dosages and who prescribes them.
- Focus on current symptoms: Focus on your client’s current symptoms that are listed in the DSM, and avoid talking too much about your client’s past or theories. Describe the severity and duration of symptoms and include scores, even if self-reported, from diagnostic tests. For example, if a client is experiencing depression due to the death of a loved one, you would say they experience insomnia and get about 4 hours of sleep per night and you would also list precipitating factors that led to the patient needing treatment. Precipitating factors are always pertinent (in both inpatient and outpatient settings) and are equally important for getting paid for the case.
- List problems with functioning: Provide specific examples of how your client’s symptoms negatively impact their life. For example, you might say your client missed a week of work in the past month due to depression.
- Identify risk factors: Discuss your client’s risk factors, such as regular alcohol or substance use and whether or not they are a danger to themselves or others. Include relevant information such as past suicide attempts or psychiatric hospitalizations.
- Explain your detailed treatment plan: Be ready to explain the details of your treatment plan, such as what you do during sessions, what you ask your client to do in their own time and how the interventions help them. Make sure the treatment plan includes measurable goals and addresses all of the diagnoses you mentioned. For example, if your client has both depression and anxiety, make sure you have treatment goals addressing both or have coordinated treatment with another provider.
- Address goals that relate to medical symptoms: Make sure to discuss goals and how they treat specific medical symptoms and avoid talking about general goals for self-improvement. For example, instead of saying a goal is to improve anxiety, you might say a goal is to decrease panic attacks from once a day to once a month. Explain how the treatment plan will help your client accomplish this.
- Find the right balance between progress and needing more treatment: An insurance company will not want to cover a client who is either not progressing at all or who is too well for treatment. Therefore, if you believe the treatment will continue to help your client, make sure to demonstrate their progress, but also be ready to prove they still need treatment and you have plans to help them progress further.
- Take a deep breath: A treatment review can feel like a nervewracking experience, especially if you know your patient’s care is on the line. If you prepare, you’ll have a much easier time staying calm during the review. Take a breath, and try to look at the review as if you’re educating the reviewer about your client’s diagnosis and treatment plan. If the insurer ultimately decides to deny the client’s care, you can appeal their decision. There are first and second level appeals and insurance companies are required to honor the request for appeals. While this doesn’t mean that the insurance company will authorize the care, they will at least “hear” the case.
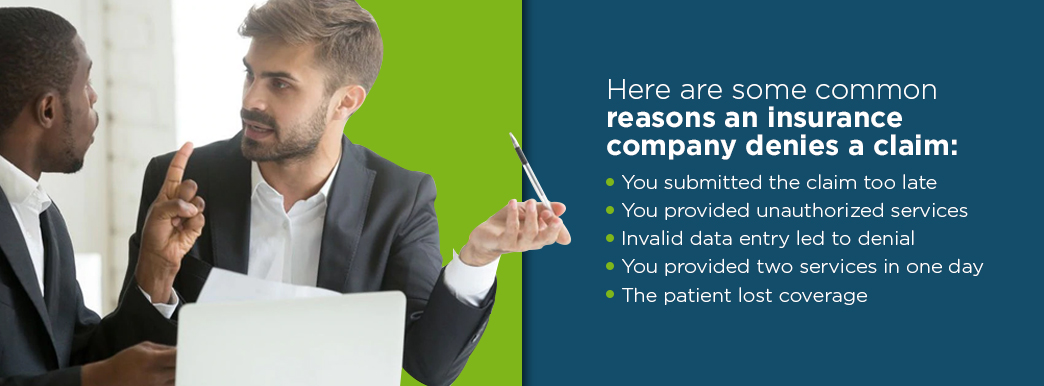
What Can I Do If My Insurance Company Denies My Claim for Reimbursement?
If your insurance claim was denied, try not to be alarmed. It’s important to first determine the cause of the denial and then take steps to fight for reimbursement. Here are some common reasons an insurance company denies a claim:
- You submitted the claim too late: While treatment facilities are able to file a “retro” review, this is not the standard and is very different from reviewing during treatment. Insurance companies may or may not cover the service for retro authorizations no matter if the service was medically necessary or not. It is best practice to complete review and process claims at the time services are rendered (pre-authorization may also be required). Treatment review dates are dependent on the insurance company and the company’s reviewer (judgment) of when the concurrent reviews take place. Some companies, for example, have a standard 3-day or 7-day period, but many are reviewed on a case-by-case basis according to the patient’s condition. Claims will be rejected if filed too long from the date of service. You can prevent this from happening in the future and get claims in on time by using an efficient integrated electronic billing system.
- You provided unauthorized services: For many insurance companies, mental health treatment must be pre-authorized (except acute inpatient care). Make sure to keep track of how many sessions or appointments you’ve provided and make sure the services have been pre-authorized. The practice’s reviewer will do this up front and will count the number of used sessions along the way as reviews are completed. In the event that a patient misses an appointment, the staff can “bargain” to receive credit for that missed session so the patient/treatment facility does not lose any sessions. If the facility does not request credit for the session, the reviewer will count it as if the patient attended and the session is lost. To request authorization for pending services, the treatment facility must contact the insurance company. (Please note that authorization for services is never a guarantee for payment.)
- Invalid data entry led to denial: Sometimes missing or incorrect patient information can lead to a denied claim. An intuitive, easy-to-use billing system can help reduce manual errors.
- You provided two services in one day: Many times, insurance companies do not cover more than one behavioral health service per day. So, even if your client is allowed several sessions, you can only provide one session per day. This can get tricky with group therapy or testing services, which may fall under the one-per-day category.
- The patient lost coverage: If a patient unknowingly loses insurance coverage or doesn’t tell you, your claim will be denied. Likewise, if they change plans you will need to be part of their network and get pre-authorization to see the client. Without either of these, the claim can be denied. Changes to the patient’s insurance coverage should all be known upfront by the treatment facility’s staff responsible for getting the pre-authorization or verification during the initial visit.
Although there are many reasons a claim can get denied, there are steps you can take to fight a denial and get compensated for your work.

How Do You Fight an Insurance Claim Denial?
Whether an insurance claim was denied due to an error or lack of authorization for services, you can still fight for reimbursement. Take these steps:
- Make a phone call: First, call the insurer. They may be able to quickly identify the cause of the denied claim, so you’ll know how to move forward.
- Speak with the manager: Ask to speak with a supervisor and see if there’s anything you can do to resolve the issue.
- Ask for the reasons in writing: If you’re not able to find a resolution after a few calls, you may decide to appeal the denial. First, ask for the specific reasons for the denial in writing and request copies of any plan guidelines that support the denial. You’ll use this information to help you construct an appeal letter.
- Write an appeal letter: You might write an appeal letter to argue against the denial or request an exception to the policy. Ask the insurer about deadlines and how the appeal process works. The American Psychiatric Association (APA) provides a sample letter to help you get started.
Even though a claim denial is not something any clinician wants to deal with, it can be part of a learning experience. Use claim denials to teach you ways to improve your denial management strategies. An efficient denial management system will help you streamline the reimbursement process and reduce future claim denials. Use the following tips to incorporate healthcare denial management in your practice:
- Understand why claims were denied: The first step in denial management is understanding why your client’s claim was denied. Once you know the reason for the denied claim, reach out to your patient and educate them about insurance claims and denials. You can work together to resolve claim issues.
- Keep claim denials organized: You don’t want to lose track of claim denials, as they can quickly pile up. Use an organized system to track, manage and resolve denials.
- Don’t wait: Have a strong workflow to handle denied claims so that when you receive a denial you’re ready to take action and correct it within a week. Part of this is being able to document and track claims easily.
- Track progress: Track progress so you can see how your practice has improved regarding denial management – and where you need more work.
- Identify trends: Consider whether claims are being denied for the same reason or if denied claims are getting lost. By identifying the most common cause of claim denials, you’ll be able to develop an effective denial management system.

Use ICANotes for Insurance Treatment Reviews
If you keep thorough, up-to-date mental health therapy notes, you’ll be prepared for a treatment review whenever one arises, and a review will be much easier to handle.
At ICANotes, we can help you keep organized, detailed therapy notes with our EHR software designed especially for busy behavioral health professionals. Our intuitive and time-saving templates streamline the documentation process. With ICANotes, you can document initial assessments with drop-down menus and minimal typing. You can also keep track of a patient’s progress, history and diagnosis with an easy-to-use progress note template – or be ready for a treatment review with our comprehensive treatment plan module. Overall, you’ll spend less time on documentation so you can spend more time caring for patients. Experience the benefits of ICANotes firsthand with a free trial, or contact us today to learn more.