Supporting Emotional Well-Being During the Coronavirus Pandemic
People across the globe are battling the whirlwind of emotions associated with the coronavirus. COVID-19 put a harsh pause on people's lifestyles, forcing them to find a new sense of "normal" in isolation. This lifestyle change has often paired with worry about the virus's spread, scope and global impact.
Teaching patients mental health coping skills to support their well-being during and post-COVID-19 is important. Without these skills, patients may rely on unhealthy coping strategies, potentially resulting in short- or long-term mental illness — even suicide in extreme cases.
Before we outline ways to support your patients' mental health during COVID-19, we want to acknowledge your passionate efforts to care for your clients. Your work is important and doesn't go unnoticed.
Table of Contents
- How COVID-19 Is Impacting Emotional Well-Being
- COVID-19 Suicide Risk Factors
- Providing Suicide Care During the COVID-19 Pandemic
- Additional Tips for Supporting Emotional Well-Being
- Visit Our Blog for More Tips
How COVID-19 Is Impacting Emotional Well-Being
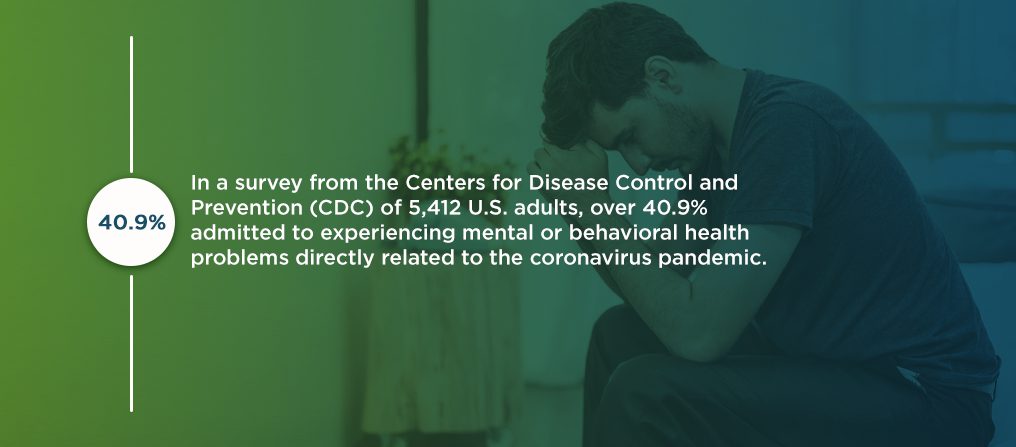
The world is facing stressful circumstances. In a survey from the Centers for Disease Control and Prevention (CDC) of 5,412 U.S. adults, over 40.9% admitted to experiencing mental or behavioral health problems directly related to the coronavirus pandemic. And, over half of the survey's respondents said they experienced symptoms of anxiety, depression and trauma- and stressor-related disorder (TSRD) — with 10.7% reported to have considered suicide.
In addition to the precautionary isolation measures, the emotional distress surrounding a new disease plays a large role in these high reports of anxiety and depression. Stress over COVID-19 can cause:
- Disruptions in sleeping patterns.
- Changes in eating patterns.
- Difficulty concentrating.
- Worsening of chronic health problems.
- Worsening of mental health conditions.
- Increased substance use.
- Persistent fear of one's health or the health of others.
Our mental health affects the way we live our lives. The way we think, interact with others, make decisions, handle day-to-day life and respond to stress are all indicators of our emotional state. Constant worry inhibits people's abilities to function, leading to short- or long-term mental illness without proper support.
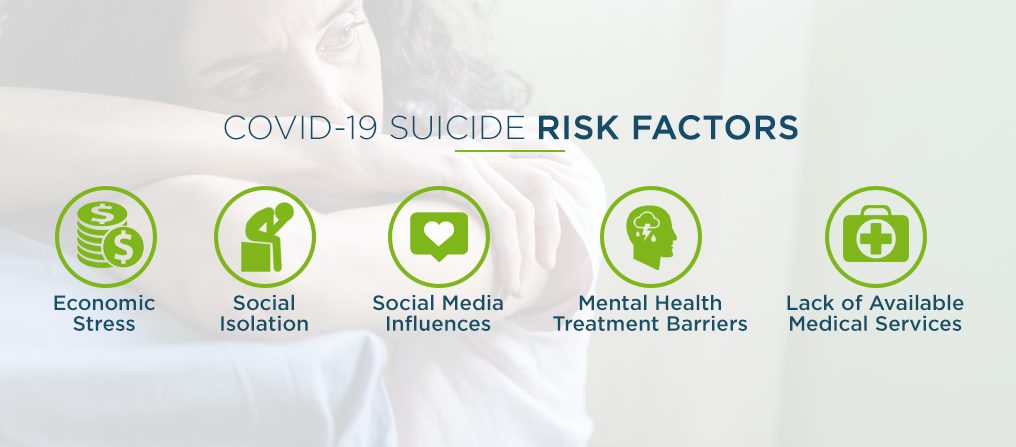
COVID-19 Suicide Risk Factors
Health care providers are appropriately wary of the increased suicide risk surrounding worsening mental health conditions. In the U.S., suicide is ranked the 10th leading cause of death, with rates steadily rising since 1999. This growing concern is enhanced due to COVID-19 factors like:
1. Economic Stress
Just weeks into the coronavirus pandemic, 20.6 million Americans lost their jobs. The U.S. hasn't seen an unemployment rate so high since the Great Depression in the 1930s, and it far surpasses the jobs lost during the Great Recession in the late 2000s.
Nobody could have prepared for the unforeseen mass job loss. Now, these millions of Americans are balancing the already-stressful circumstances surrounding the global pandemic with financial anxiety caused by depleted savings accounts, lack of stable income and inability to pay off debts.
2. Social Isolation
The precautionary measures established to reduce the spread of the coronavirus, namely social distancing and quarantining, challenge the way patients socialize with their support groups. Face-to-face interactions are shown to reduce symptoms of depression and other mental health problems, but this type of socializing is now difficult to do.
Patients with anxiety and depression can feel like they're battling their thoughts. This is especially true when faced with mental health issues and isolation, where patients are more likely to fall victim to a vortex of negative thoughts and ruminate on the worst-case scenarios.
Being unable to take a break from these intrusive thoughts through social interaction can make patients feel like they're losing a battle. This problem leads to worsening mental health symptoms and, ultimately, a higher risk of suicide.
3. Social Media Influences
As fear and anxiety about the coronavirus spread, people turn to social networking sites to share and find information in hopes of gaining peace of mind or insight. This phenomenon birthed what some people are calling the first social media "infodemic."
Social networking sites seem to have no boundaries, sharing misinformation and creating even more widespread panic about COVID-19. Studies show that this is especially true in people between 18 and 35 years old, who report using social media more than other age groups and face higher levels of psychological anxiety.
4. Mental Health Treatment Barriers
As more people face mental health challenges, mental health services are met with a dramatic influx in patients. Unfortunately, this means many mental health service providers reached full capacity, leaving people discouraged and forced to rely on suicide hotlines and telehealth services as their only means of treatment.
Crisis lines, like the National Suicide Prevention Lifeline and Disaster Distress Helpline, have experienced a dramatic increase in calls since February — up to 338%. In the last three weeks of March, a St. Louis hotline reported they received 396 callers struggling with suicidal thoughts, 16% of which mentioned COVID-19. The next month, that number jumped to 1,018 callers, with 34% labeling COVID-19 as their main trigger.
Despite these downsides, the coronavirus is inspiring a revolutionary change for the future of mental wellness. Health care providers are meeting this influx by stripping barriers and making psychological care more accessible when people need it most.
5. Lack of Available Medical Services
Hospitals and health systems labeled treating COVID-19 as their number one focus, canceling non-emergency procedures and disrupting supply chains to meet the growing demand for coronavirus care and prevention.
Although undeniably important, this health care shift significantly impacts those who struggle with chronic medical problems, among other patients who require regular medical care. Patients with chronic medical conditions are more likely to experience suicidal thoughts, and being unable to receive treatment for these conditions can amplify anxiety, stress and feelings of hopelessness.
Providing Suicide Care During the COVID-19 Pandemic
When caring for clients, be aware of the potential of COVID-19 evoking suicidal thoughts in your patients. Prepare yourself with the right knowledge and precautionary measures to help them through their feelings safely.
Who Is More Likely to Be Impacted by COVID-19?
Although the coronavirus pandemic affects everyone, some people's emotional well-being is more likely to be impacted than others. Patients may respond differently to the coronavirus depending on their background, support group and physical and emotional health pre-COVID-19, among other factors.
According to a CDC survey, people who are more likely to report worsening mental or behavioral health symptoms include:
- Younger adults.
- Racial minorities.
- Essential workers.
- Adult caregivers.
Unpaid adult caregivers have the highest likelihood — 3.33 times the odds — of reporting anxiety, depression or post-traumatic stress disorder (PTSD) symptoms than any other group. However, respondents between the ages of 18 and 24 are the most susceptible to serious suicidal ideation.
What Are the Warning Signs of Suicide?
Aside from demographic statistics, other warning signs indicate your patient may be struggling with suicidal thoughts. As you work with your patient, note possible warning signs, such as:
- Talking about death or suicide.
- Obtaining lethal means, like a firearm or an accumulation of pills.
- Isolating themselves from loved ones.
- Experiencing dramatic mood swings.
- Expressing feelings of hopelessness.
- Excessively using alcohol or drugs.
- Giving away belongings without the need to do so.
- Saying goodbye to loved ones.
If you recognize these warning signs in your patient, develop a strategized plan to support their emotional well-being and, most importantly, keep them safe.
What Should You Do If Warning Signs Are Present?
First, don't panic. If you notice these warning signs, or if your patient openly talks about having suicidal thoughts, consider it a giant leap toward recovery. Listen to how they're feeling and try to identify their largest concern, then follow these five steps:
- Acknowledge their concerns and validate their feelings: Acknowledge their strength for opening up to you, and validate their feelings by recognizing the nature of their worries.
- Redirect their feelings: The alarms in your patient's head are sounding, and they need help turning them off. Redirect their emotions away from the thought vortex and toward a healthier, safer thought process.
- Educate them on healthy coping mechanisms: Empower your patient to take control of their thoughts by teaching them more beneficial ways to cope with their concerns. Doing so fortifies their long-term safety and allows them to restructure their thoughts by themselves in the future.
- Create a safety plan: Now that the alarms are off, work with your patient to create a safety plan. Take the coping mechanisms you discussed and urge your patient to write them on paper. Encourage them to keep their safety plan with them and involve their support group to strengthen their ability to help.
- Reduce access to lethal means: As a part of the safety plan, address your patient's access to lethal means, such as medications or firearms. Limiting their access to these objects and substances is important, and it is admittedly one of the more challenging aspects of helping suicidal patients.
Above all, your goal is to bring hope — the key to suicide prevention — back to your patient.
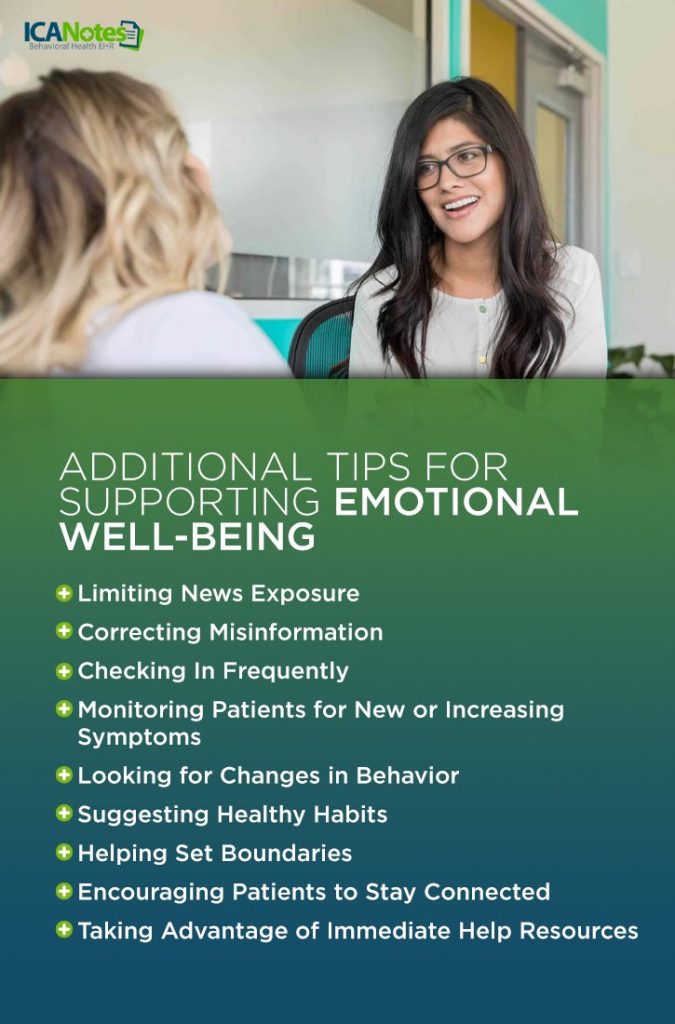
Additional Tips for Supporting Emotional Well-Being
Feelings of isolation, depression, anxiety and other stressors accompanied by COVID-19 are known to raise the risk of suicide. Some ways you can reduce these feelings and support your patients' emotional well-being are:
1. Limiting News Exposure
Patients should stay informed about the coronavirus. However, being surrounded by mass 24-hour coverage makes it difficult for people to turn their attention away from the constant stress and worry. Continuous COVID-19 news exposure prevents patients from dedicating their full attention to their mental health.
2. Correcting Misinformation
Patients should also stay informed on the facts, not rumors. False information weaves its way into factual material on social media sites and through verbal communication, which can spark even more stress and fear in individuals.
Direct your patients to credible public health resources, like the Centers for Disease Control and Prevention and the World Health Organization (WHO).
3. Checking In Frequently
Check in with your patients regularly — especially those with suicidal ideations. You can do this with your patients via:
- Email.
- Social media.
- Text.
- Phone call.
- Video call.
- Other mobile apps.
Checking in with your patient personalizes your health care approach, making them feel cared for and encouraged to keep practicing beneficial mental health techniques.
4. Monitoring Patients for New or Increasing Symptoms
Monitor your patients' symptoms during your check-ins and routine appointments. Revisit the warning signs for suicide, anxiety, depression and isolation, and watch for new or amplified symptoms in their speech and behavior.
5. Looking for Changes in Behavior
Your patients' behavior can change for numerous reasons, including new or increasing symptoms, alcohol or drug use or an undiagnosed mental illness. Some behavioral changes you should look for are:
- Confusion.
- Delusions.
- Disorganized speech.
- Hallucinations.
- Mood extremes.
These behavioral changes may indicate poor coping strategies or added stressors within your patients' lives that you can discuss and work through.
6. Suggesting Healthy Habits
Following the coronavirus outbreak, patients have had to develop and adjust to completely new daily routines, which may consist of unhealthy coping mechanisms. Encourage your clients to establish new daily schedules full of healthy habits, like:
- Going to bed at the same time every night.
- Getting the appropriate amount of sleep.
- Waking up at the same time every morning.
- Journaling.
- Eating healthily.
- Exercising regularly.
- Avoiding excessive alcohol and drug use.
- Finding a hobby.
- Connecting with faith-based organizations.
Restructuring a daily routine can prove challenging, so offer your patients continual support as they work toward adopting these new habits.
7. Helping Set Boundaries
Patients may feel a heightened need to keep their loved ones safe and protected against the coronavirus. Although these are well-meant intentions, excessive thoughts can lead to obsessive thinking patterns and poor self-help.
Inform your patients of how they can limit these thoughts, as well as ways to set healthy boundaries with loved ones — and themselves — for talking about the coronavirus.
8. Encouraging Patients to Stay Connected
Isolation is a large contributor to worsening mental health conditions. Encourage your patients to stay connected with their loved ones while practicing safe precautionary measures. Your patients can connect with their support group through ways like:
- Phone calls.
- Text messages.
- Video calls.
- Emails.
- Letters.
- Online video games.
In addition to staying in contact with loved ones, make sure your patients know how they can reach you outside of scheduled appointments in case of emergency.
9. Taking Advantage of Immediate Help Resources
Supply your patients with immediate help resources. The factors surrounding the coronavirus pandemic increase the chances of suicidal thoughts, domestic violence, child abuse, sexual assault and other crises.
Some suicide prevention resources and other immediate help systems you can supply your patients with include:
- National Suicide Prevention Lifeline: 1-800-273-TALK (8255) for English,or 1-888-628-9454 for Spanish. Patients can also reach this resource at Lifeline Crisis Chat.
- Disaster Distress Helpline: 1-800-985-5990, press 2 for Spanish. Or, patients can text "TalkWithUs" for English or "Hablanos" for Spanish to 66746.
- Veterans Crisis Line: 1-800-273-TALK (8255). Patients can also reach this resource via Crisis Chat or text at 838255.
- National Sexual Assault Hotline: 1-800-656-HOPE (4673). Patients can also reach this resource via Online Chat.
- National Child Abuse Hotline: 1-800-4-A-Child (1-800-422-4453), which patients can also text.
- National Domestic Violence Hotline: 1-800-799-7233, or patients can text "LOVEIS" to 22522.
- The Eldercare Locator: 1-800-677-1116.
Mental illness is a chronic struggle for patients, and their support group may not be available when they need them most. By supplying patients with these immediate help resources, they'll always have access to potentially life-saving support.
Visit Our Blog for More Tips on How to Support Your Patients' Emotional Well-Being
Behavioral health clinicians and organizations are essential now more than ever. ICANotes recognizes your monumental efforts to support your patients' well-being during these challenging times. With our electronic health record (EHR) software, we aim to save you time and keep you organized so you can keep up with your patients' changing needs.
Visit our blog to learn more about how our EHR software can help you — plus other ways you can support your patients' emotional well-being during COVID-19.
Related Posts:
The Impacts of COVID-19 on Mental Health
COVID-19 and Your Therapy Practice
How to Make Your Practice Virtual
Telehealth Care Becomes More Accessible Amidst the COVID-19 Pandemic