What They Don’t Teach You in School About Clinical Documentation
Concise clinical documentation can lead to excellent recovery results for patients, but can be disastrous if not done well. When you're in a field with the potential to change lives, it's essential to make sure all elements of your written work are clear and factual.
Let's look further at the significance of clinical documentation, the consequences of incorrect recordkeeping, typical medical documentation errors and clinical documentation tips.
Table of Contents
- The Importance of Clinical Documentation
- The Consequences of Incorrect Clinical Documentation
- The Most Common Medical Documentation Errors
- Clinical Documentation Guidelines
- Make Clinical Documentation Easy With ICANotes
The Importance of Clinical Documentation
Clinical documentation is essential for many reasons, but let's begin by looking at two.
Standard of Care
The healthcare industry has established legal standards surrounding a patient's right to quality care. These can come in the form of protocols and procedures, internal policies, professional association and accreditation standards and federal or state statutory or regulatory requirements. If a health provider doesn't adhere to these principles by not keeping detailed notes, they may encounter severe consequences.
Licensing
A health provider found liable for keeping incorrect clinical documentation may face investigation of complaints, hearings or disciplinary sanctions. The outcomes of inaccurate or incomplete clinical documentation can also include a physician's license being revoked or suspended.
Medical staff bylaws and Joint Commission standards strive to promote quality patient care. Correct clinical documentation is part of complying with these standards. An internal review is one potential repercussion of noncompliance.
The Consequences of Incorrect Clinical Documentation
Clinical documentation is how healthcare workers keep track of multiple patients' records and medical history. If something goes awry with these files, it can adversely affect a patient's health.
Wrong Diagnosis
Some diagnoses share similar symptoms, which is why it's vital to accurately keep track of a patient's medical history, their complaints and what medications they're taking. For example, lupus can lead to kidney failure, but so can other diseases. If you happen to document results from a patient's blood test incorrectly, you may miss that they have lupus, and the patient may not get the treatment they need for it, such as steroids or even surgery.
Wrong Medication
Various people react to medication differently due to their unique genetic makeup, metabolism or interactions with other drugs they take. For example, health providers commonly suggest that people with high blood pressure should not use ibuprofen. Let's say you forget to mark down that someone has a history of high blood pressure, and you tell them to take ibuprofen every day. This patient is then at risk for their blood pressure medication not being as effective as it needs to be.
Adverse Reaction to Medication
A patient can have an adverse reaction to medication due to something else they're taking or because they have another disorder that may interact with their medicine. For instance, if you fail to note that a patient is already on an SSRI, and you prescribe them a second SSRI, you put them at risk for serotonin syndrome and possibly even death if not treated quickly.
Injury or Death
As a medical worker, you want to save people's lives and prevent suffering, but even small mistakes in clinical documentation can lead to a patient's injury or death. For example, if you switch two patients' charts, and one patient has a failing heart, they might not get the care they need in time to save them.
The Most Common Medical Documentation Errors
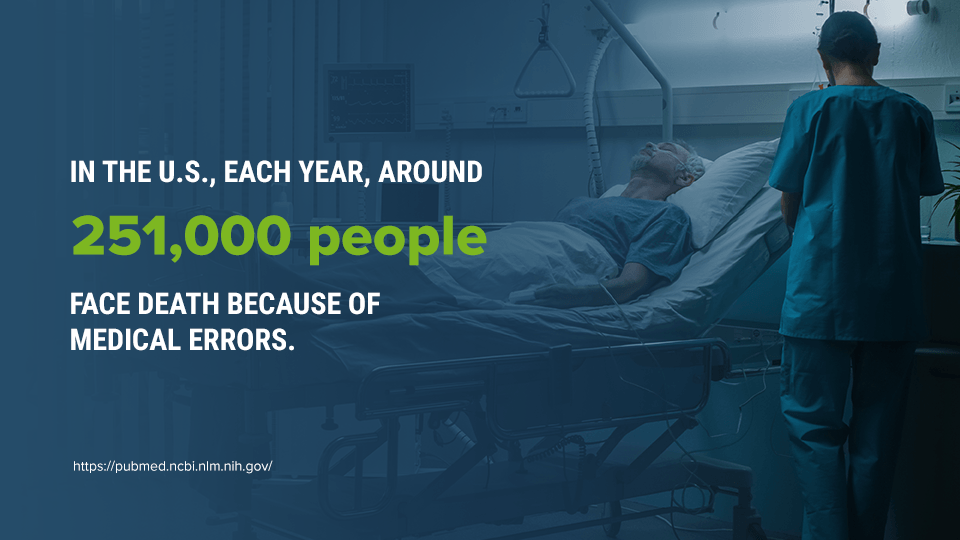
Medical documentation errors can lead to consequences for you and your patients, and they're not as rare as you might think. In the U.S., each year, around 251,000 people face death because of medical errors.
Sloppy Handwriting
Handwriting can be personal, but making an effort to neaten your sloppy handwriting could profoundly affect your patients' care. Imagine a doctor is reviewing a patient's notes to understand their medical history. If they cannot read pertinent information or misinterpret a detail, this could be disastrous.
Some diagnoses have similar spellings, like hypothyroidism and hyperthyroidism. If illegible handwriting causes someone to mistake one disorder for another, the patient won't get the remedy they need or may even get care that further harms them.
You can eliminate the problem of messy handwriting with software solutions like ICANotes.
Typos and Copy+Paste Errors
Copy and pasting a portion of a patient's record into a new program or file may seem like a smart way to save time and keystrokes. Still, there's a risk that some information may not get copied and pasted in the correct order, or that other details might get left out.
Also, copying and pasting information may lead to a medical worker reusing old notes instead of making detailed notes of their own. This practice may lead to a lack of knowledge further down the line about a patient's medical history or how their diagnosis has progressed.
Wrong Abbreviations
In the fast-paced medical world, abbreviations are essential. However, it's best to stick to standard shorthand. If you make up new abbreviations, consider creating a legend for them and keeping several copies of it around the office.
Some abbreviations can be easy to confuse for one another. For example, q.d means a patient should take medication once a day, and q.i.d means a patient should take medication four times a day. Using one of these abbreviations in the place of the other could lead to a patient overdosing or not getting enough medication to treat their condition effectively.
Entering Incorrect Information Into the Chart
As a healthcare worker, you've likely overseen treatment plans for a large volume of people. It's easy to get patients confused, especially when you're mentally fatigued. This mistake can have severe consequences for a patient's health and well-being. Be alert and double-check your notes to avoid mixing up patients with similar diagnoses, names or physicians.
Documenting Conflicting Information
It stands to reason that some information in a patient's file may end up in the wrong section, especially if there is no standardized template used across a workplace. If notes end up misplaced, a patient's overall medical history may seem confusing. For example, your record might make it seem as if a long-ago surgery was much more recent. This error will muddle a patient's medical history and may lead to them receiving incorrect care.
Failing to Sign, Date and Time a Medical Entry
Knowing who provided care and when is vital in understanding a patient's file. If these details are wrong or misleading, the patient may end up getting care from someone who does not specialize in their condition, or have their next appointment set up sooner or later than it should be.
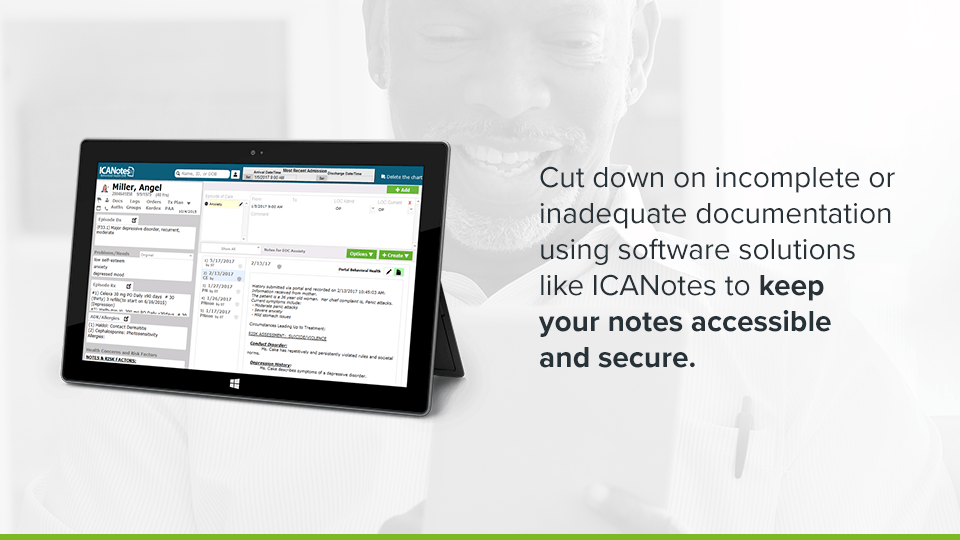
Incomplete or Missing Documentation
Unfinished or fragmentary details can be a hazard for those who must be familiar with a patient's medical history, symptoms and current medication. Imagine if someone ends up writing notes on the wrong chart or failing to provide an accurate description of the patient's condition. This carelessness could lead a different provider to prescribe or administer medications incorrectly. The ramifications of mistakes like these can be severe, including malpractice lawsuits and the patient's illness or death.
Cut down on incomplete or inadequate documentation using software solutions like ICANotes to keep your notes accessible and secure.
Failing to Document Omitted Medications and Treatments
When you don't document any changing information about a patient, such as their past treatments, allergies and current medications, you're putting yourself and anyone else involved with a patient at risk of being liable for negligent patient care.
More importantly, your patient may suffer due to a caregiver failing to document omitted medications and treatments. Even minor changes in a patient's medical history need accurate documentation to ensure their correct care in the present and future.
Neglecting to Document Drug Reactions or Changes in a Patient's Condition
Of course, you need to notice and respond to drug reactions or changes in a patient's condition. However, you must also document them. Any other professionals who treat your patient need a comprehensive view of their medical history.
Remember, various patients will react to drugs differently. Be cautious, and describe any changes you may see in your patient after administering a new treatment.
Failing to Document Noncompliance
When you fail to document noncompliance on a patient's part, you open yourself up to liability and accusations of abandonment. For example, a patient might miss several appointments, refuse to be screened for a diagnosis or ignore their prescription instructions. You must document all these instances of noncompliance.
Adding Entries Later On
When you add entries a while after you meet with a patient, you risk forgetting small but critical details about the patient's symptoms and medical history. You don't often get the opportunity to talk with a patient again before you draw up and administer their treatment plan, so it's vital to get things right the first time.
Documenting Subjective Data
Stick to the facts when making clinical documentation. For example, you may notice a patient looks sad, but writing that they have depression when they lack an official diagnosis may complicate their treatment in the future.
Only Charting the Abnormal
As a healthcare professional, you probably get positive and negative results when screening patients. It's crucial to document both. If you only note the positive findings, you run the risk of running repetitive tests down the line if your treatment plan ends up being less effective than you anticipated. Remember, negative outcomes are often valuable in ruling out different diagnoses.
Clinical Documentation Guidelines
Let's look at some helpful guidelines you can follow when trying to improve your clinical documentation skills.
Use Software
Using healthcare management software can help save you time and keep patient information secure while allowing you to work efficiently and intelligently. For example, ICANotes lets you schedule, communicate, document and bill all in one place from anywhere. Using software will also keep all your notes according to the same standards because they will follow templates you establish. Save time typing and spend more time caring for your patients.
Write Consistent Notes
Make it your mission to write the same kind of note for different types of patients. Strive to be detailed in your note writing, regardless of your patients' medical history, insurance coverage or age. All your patients deserve quality care, and that starts with detailed, clear and concise note writing.
Be Precise
Precise note writing involves being strict with yourself on describing a patient's exact symptoms and medical history in as much detail as possible. For example, imagine you suspect a patient has heart failure, so you decide to run some tests.
Because you're already proceeding with the tests, you decide to skip describing the patient's symptoms and medical history. What if the patient's condition changes before you finish testing, and you have to go back to the drawing board? It may be challenging to remember information if you never wrote it down.
Make Clinical Documentation Easy With ICANotes
ICANotes can help take your note writing to the next level by allowing you to create detailed notes and mental health records without having to type or dictate. Overall, you can schedule appointments, bill, report and e-prescribe with our software.
ICANotes offers the following benefits:
- Reduced documentation time
- Compliance with Medicare and Medicaid requirements
- No more transcription expenses
- Minimized medical-legal risk
If you want to know more about what we can do for you, request your free trial today, or give us a call at 866-847-3590.
Sources
- https://www.wolterskluwer.com/en/expert-insights/nursing-documentation-how-to-avoid-the-most-common-medical-documentation-errors
- https://www.mosmedicalrecordreview.com/blog/common-medical-documentation-errors-that-could-prove-costly/
- https://bok.ahima.org/doc?oid=107687#.YU3NaJrMIYp
- https://www.ncmic.com/insurance/malpractice/risk-management/common-documentation-mistakes/
- https://www.chirohealthusa.com/consultants/the-10-most-common-ehr-documentation-errors/
- https://www.nso.com/Learning/Artifacts/Articles/7-Common-Pitfalls-to-Avoid-in-Charting-Patient-Information
- https://www.nso.com/Learning/Artifacts/Articles/7-Common-Pitfalls-to-Avoid-in-Charting-Patient-Information