CMS 1500 Claim Form Instructions
A CMS 1500 form is a claim form you will often use in private practice behavioral health care. This form bills Medicare carriers and in-network insurance providers for the reimbursement of some eligible services you provide for patients. You will fill these forms out any time you want to submit an insurance claim. While you can submit them by mail with printed versions, most providers allow electronic submissions for more efficient processing.
If you're unfamiliar with how to complete this form, keep reading to see a dissection of the CMS 1500 claim form instructions and learn how to avoid common mistakes.
Table of Contents
- Why You Don't Want to Make Mistakes When Submitting the CMS-1500
- What Information to Include
- Common Mistakes on CMS 1500 Forms
Why You Don't Want to Make Mistakes When Submitting the CMS-1500
There are about 33 items to fill out on the CMS 1500 form — but not all are required for every patient or type of service. You will leave some fields blank depending on a few different factors because every patient, coverage and service is different. It can be easy to miss something or enter inaccurate information if you don't already know how to complete a CMS 1500 form because there are many fields to fill out.
However, even the slightest mistake can cost you money, delay your processing time or even deny your reimbursement. You will have to pay to correct and resubmit your form every time insurance companies reject or deny it, which cuts into your profit margin. Learning how to properly fill out and submit your billing forms can help you maximize your reimbursement rate and leave you with less hassle.
What Information to Include
It can be challenging to know what information to include on your CMS 1500 form — especially if you've never filled it out before or have to do it often and forget certain steps. Here's a breakdown of the CMS 1500 claim form instructions that highlight the required information, fields to leave blank and items that may or may not apply to your service or patient.
Insurance Details
The very first steps on your CMS 1500 are to fill out insurance coverage information in steps 1 and 1a:
- Coverage: Indicate the type of health insurance coverage that applies to the claim, such as checking the Medicare box.
- Insured's ID number: The patient and the insured may not always be the same person. List the insured's identification number and verify that it corresponds to the insured's name information on step 4. This step is required.
Patient and Insured Information
The next few sections will ask you to fill out some specific information about the patient and the insured person — if they're different people — so make sure their details are correct in your system and paperwork. For these next steps, you'll need the following information:
- Patient's name, birth date and gender: Enter patient's full last and first names and middle initial. If they have a suffix, enter it between the first and last names. Enter the birth date in the MM/DD/CCYY format and mark an X in the box for the patient's sex.
- Insured's name: List the insured's name in the same format as step 2.
- Patient's address and telephone number: Enter the patient's mailing address and telephone number without any punctuation. You can use a hyphen for a nine-digit ZIP code only.
- Patient's relationship to the insured: Check the appropriate box for the patient-insured relationship according to the information on steps 2 and 4.
- Insured's address and telephone number: Enter the insured's address unless it's the same as the patient's address in step 5. If so, write “SAME” in this field. Complete this step only after you enter step 4 and 11.
- Patient status: Check the appropriate box for the patient's student, employed and marital status.
Sections 9-13 primarily focus on the insured's information — apart from the patient's signature on step 12. For these next steps, you'll need the following information:
- Other insured's name: Fill out field 11d first — if marked “yes,” then enter the full name of the person insured under another payer in field 9.
- Other insured's policy or group number: Fill out field 11d first — if marked “yes,” then enter the other insured's policy/group number or ID number in field 9a.
- Other insured's date of birth: Fill out field 11d first — if marked “yes,” then enter date of birth in MM/DD/CCYY format and mark an “X” in the box to indicate gender in 9b. If gender is unknown, leave blank.
- Other insured's employer's name or school name: Fill out field 11d first— if marked “yes,” then enter insured's employer or school.
- Other insured's insurance plan name or program name: Fill out field 11d first — if marked “yes,” then enter the insured's company or program name.
- Is the patient’s condition related to employment, auto accident or other accident?: Mark the appropriate box for each question if the patient's treatment or service relates to employment or any type of accident. If “yes,” for an auto accident, include the state postal code.
- Reserved for local use: Leave this field blank — it is not required.
- Insured’s FECA number or policy group: Add the policy or group number according to the insured's healthcare ID card.
- Insured's gender and date of birth: Enter birthdate in the MM/DD/CCYY format and gender if different from step 3.
- Employer name or school name: If applicable, add the insured's employer or school name.
- Insurance plan name or program name: Add the insured's insurance company or program name.
- Is there another health benefit plan?: Mark the box accordingly if there is other insurance involved in the reimbursement of the claim.
- Patient's or authorized person's signature: If the patient is authorizing the release of their medical information, they must sign and date the claim before processing. Their signature also authorizes payment of benefits to the service provider.
- Insured’s or authorized person’s signature: You can use a signature on file (SOF) to authorize payment of benefits to the provider. Leave blank if there is no SOF.
Provider Information
Items 14-23 focus primarily on your information as the provider for these services. For this next section, you'll need to include the following information:
- Dates patient unable to work in current occupation: Fill out this field if the patient is eligible for worker's compensation or disability benefits using the MM/DD/YY format.
- Name of referring physician or other source: Enter the name if applicable.
- ID number of referring physician: Use the CMS-assigned seven-digit UPIN for the referring provider in step 17.
- NPI: Enter the National Provider Identifier (NPI) for the referring provider in step 17.
- Hospitalization dates related to current services: If the claim includes charges for services under an inpatient admission, enter the dates in the MM/DD/YY format.
- Reserved for local use: Enter “IOP” in this field if billing for intensive outpatient programs.
- Outside lab/charges: Enter any charges processed by any other lab than the providers'.
- Diagnosis or nature of illness or injury: List an ICD-10 diagnosis code to the highest level of specificity and the services rendered. You'll use ICD-10 since your claims will likely have service dates after Oct. 1, 2015. Write “0” in the ICD Ind. field.
- Medicaid resubmission code/original reference number: Enter the reference claim number for any resubmitted claims.
Hospitalization and Billing Information
This last section of the CMS 1500 instructions is where it can get tricky because it involves all the details about your patient's procedure and billing number. Be sure to double-check these fields to ensure you're entering the correct patient and provider details accordingly:
- Dates of service: Enter the “from” and “to” dates in the MM/DD/YY format. If services only lasted one day, list it in the “from” field.
- Place of service: Enter the appropriate place of service code.
- Procedures, services or supplies CPT/HCPCS: List the valid HCPCS or CPT codes — and modifier, if applicable — for each service.
- Diagnosis pointer: List the diagnosis code reference number from step 21 to relate to the procedures performed and date of service — this is not the ICD-10 code.
- Charges: List the provider's billed charges for each service.
- Days or units: Enter the number of days or units that correspond with step 24a.
- EPSDT family plan: Mark this field only if the service was part of an EPSDT panel.
- ID. Qual.: Fill out this field if there is no NPI and add the qualifier and identifying number in the shaded area.
- Rendering Provider ID. #: Add the NPI number in the unshaded area.
- Federal Tax ID number and type: Enter the Social Security Number (SSN) or Employer Identification Number (EIN) and mark the box that identifies the type of number used for the services.
- Patient's account number: Enter your patient's unique account number.
- Accept assignment?: Mark an “X” in the appropriate box to show whether your practice accepts Medicare benefit assignments.
- Total charge: List the total charges for this claim for each service provided in step 24f.
- Amount paid: Enter the total amount the patient paid for services on this claim.
- Balance due: List the total balance due for these services left over from the amount in step 29.
- Signature of physician or supplier including degrees or credentials: Add your signature, licensure level, credentials and date of signature.
- Name and address of facility where services occurred: List the name and address where the services took place.
- NPI: Enter the NPI of the service facility.
- Physician’s/supplier's billing name, address and phone number: Enter the appropriate billing information.
- PIN: Enter the NPI of the billing provider or group.
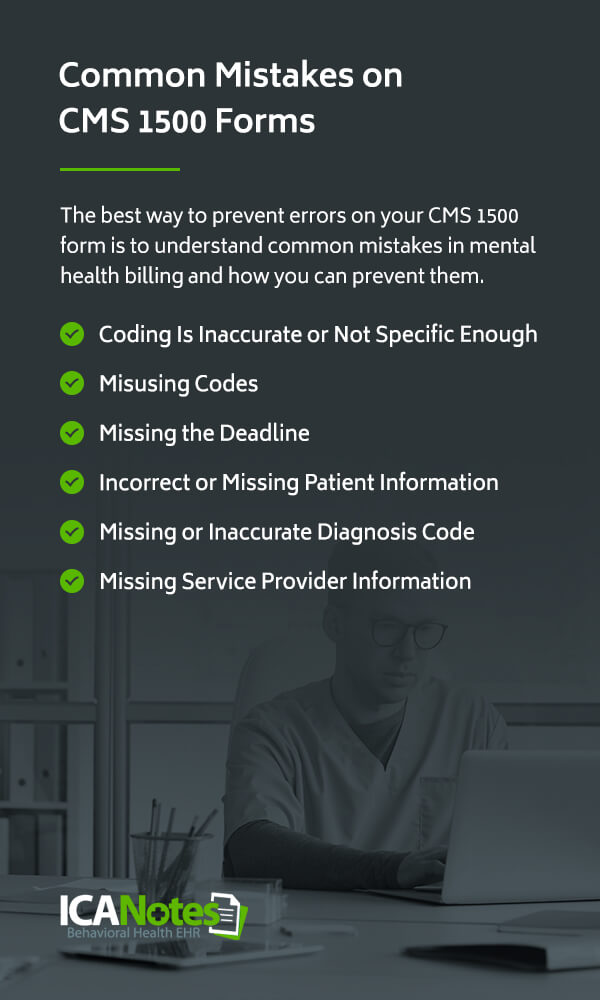
Common Mistakes on CMS 1500 Forms
The best way to prevent errors on your CMS 1500 form is to understand common mistakes in mental health billing and how you can prevent them. This practice will help minimize your rejections and denials. Let's take a look at six mistake examples for CMS 1500 forms.
1. Coding Is Inaccurate or Not Specific Enough
Use the proper diagnosis code that describes your patient's diagnosis, complaint, symptoms or condition. You may use the same codes frequently, so check the descriptions every time to ensure they match. Make sure your coding is as specific as possible, and always include applicable modifiers with your service codes. Incorrect codes can result in overbilling, underbilling, rejection and denial. Be sure to keep up with coding changes, as well.
2. Misusing Codes
Misusing codes can appear as fraud to increase your reimbursement even when it's likely an accident. You can misuse codes in two common ways:
- Unbundling: Billing for two services separately when you can use a single code for both services
- Upcoding: Billing with an inaccurate code with a higher reimbursement rate, such as spending 30 minutes in a session and using a 60-minute service code
3. Missing the Deadline
Filing your claim within a certain timeframe is just as important as filing it correctly. Some payers will request a 90-day, six-month or year timeframe, so always check that you’re billing within those periods to avoid a denied claim. As a best practice, try to bill within 30 days and ensure you submit any required supporting documentation for your reimbursement.
4. Incorrect or Missing Patient Information
If your patient information is missing — such as their name, address or relationship to the insured — payers will deny your claim. Even if you complete your patient steps, you may have entered outdated information, which will also result in a denial.
To help prevent this, always ask your patients to update their personal information once or twice a year and double-check that you’ve filled out every step before submitting. It’s also important to confirm you’ve spelled everything correctly.
5. Missing or Inaccurate Diagnosis Code
When filling out the diagnosis code that describes the signs, symptoms, complaints and conditions of your patient, always list your code to the highest level of specificity. Using a general diagnosis code will result in a denial. Payers will also deny your claim if you’re using an outdated coding book or accidentally enter the wrong code, resulting in a loss of revenue. It’s also important to submit your documentation along with your code, otherwise, there’s no way to prove you performed the services.
6. Missing Service Provider Information
Just as with patient information, leaving your service provider information blank can also result in a rejection or denial. Verify your NPI and taxonomy code are correct, and if you’re billing under a group of therapists, include your practice NPI and practice tax ID. The NPI tells the payer who provided the service, and the taxonomy code tells them what kind of provider you are, so be sure to include this information.
To get more familiar with the form before you fill it out, here's a CMS 1500 form sample you can download and view to help you with completing and processing.
ICANotes Can Help
Medical billing for behavioral health can be challenging. From documenting your notes to coding and keeping up with compliance regulations, it's easy to make mistakes. With ICANotes, you can manage many different aspects of your practice in one intuitive solution to meet your needs and streamline your processes.
With combined comprehensive charting, electronic billing and practice management, ICANotes helps you receive fewer claim rejections and denials and gain an enhanced workflow that benefits you and your patients. Start your free trial today or schedule a live demo to see how our features can help your therapy and behavioral health services.
Sources:
- https://www.cms.gov/medicare/billing/electronicbillingeditrans/1500
- https://www.cms.gov/regulations-and-guidance/guidance/manuals/downloads/clm104c26pdf.pdf
- https://www.cms.gov/Medicare/Coding/ICD10
- https://www.cms.gov/Medicare/Coding/place-of-service-codes/Place_of_Service_Code_Set
- https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/837p-cms-1500.pdf
- https://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/downloads/cms1500.pdf