Top 8 Things to Include in Your Substance Abuse Notes
Substance abuse notes are a key component of offering addiction treatment services to your patients. These progress notes contain important information about your patient that allows you to modify or adjust your treatment plan when needed. As a therapist or counselor, you’re likely very familiar with the process of note writing and the necessary role it plays in helping you track your patient’s progress.
Clear, organized notes make it easier to provide effective treatment options and refresh your memory every time you meet with your patient. But how can you tailor your notes to specific mental health needs and conditions, such as substance abuse? We’ll discuss how to write substance abuse notes with specific examples to keep them relevant and concise.
Table of Contents
What Are Substance Abuse Counseling Notes?
Substance abuse counseling notes are similar to any other type of counseling note, except they focus primarily on clients and patients who experience substance abuse issues, their treatment and progress as they undergo therapy. Substance abuse counseling notes should be purposeful, thorough and accurate and include information that explains:
- The details of why you're providing specific services for your patient
- How they're responding to care
- Their progression path
- Treatment adjustments
- Major life events or trauma
Reflecting on a session and the client's progress or barriers to progress can make it easier for therapists to provide more effective treatment. While counseling notes are essential for you as a therapist, they are also an integral part of the client's journey as they progress through various levels of care.
Depending on your practice, you may be able to share your notes with your patient, which can help them visualize their own progress and help prevent them from repeating past behavior. Sharing notes can also help you form a stronger patient-therapist relationship and encourage your patient to engage more in their treatment. You may also be able to share your notes with other clinical staff if necessary to communicate about your patient's overall care and substance abuse treatment plan.
What to Include in Substance Abuse Counseling Notes
There are many different ways you can write substance abuse counseling notes. Updated, consistent notes can help you reference past sessions or events with your patient and keep track of all necessary details to provide them with the best care possible.
Using the SOAP method, for instance, your notes would align with the following format to keep details organized:
- Subjective
- Objective
- Assessment
- Plan
Let's look at the top eight elements to include in your substance abuse counseling notes. Keep in mind that these notes may differ depending on your practice's requirements.
1. Session Information
In most types of notes you write as a therapist, it's critical to include general information about your client and session so you can easily organize and find your notes when needed. Some details you might include in your substance abuse counseling session note include:
- Patient name
- Reason for visit
- Date
- Length of session
- Client’s history and current presentation
- Developments or progress from previous sessions
- Observations about the patient
- Review of the treatment plan
- Details of the session
- The primary focus of the session
- High-risk information or safety of client
- Homework assigned or action items
- Provider questions
2. Diagnostic Summary/Behavioral Definition
In this section of your counseling notes, include your patient's medical or substance abuse history as well as any mental health conditions. Write down their diagnosis and any patterns of behavior that illustrate this disorder or condition. In your behavioral definitions, include information you gather during your therapy assessments. These details could include a few sentences about your client's reasons for seeking treatment or problem areas they want to focus on that relate to their diagnosis.
Some examples of behavioral definitions could be:
- Patient experiences continued substance abuse despite ongoing financial, social, physical and relationship problems as a direct result of the substance abuse.
- Patient demonstrates a persistent pattern of alcohol or substance abuse, manifested by increased tolerance and frequency.
- Patient reports suspending important occupational and social activities that interfere with their ability to use.
3. Problem List
This section of your notes should outline the specific issues, barriers to progress, reactions and experiences your client has had throughout their treatment and therapy overall. By highlighting the issues they're experiencing, you can refer to your notes and instantly know what you want to target during each session.
Be sure to note the relevant signs and symptoms that illustrate these problems or concerns. For example, this section might include:
- Problem: Inability to minimize substance abuse or alcohol intake
- As evidenced by: DUI arrest last month and drinking heavily more than three times per week
4. Goals
Once you identify the main problems and concerns your client has, you can move on to solutions in your counseling notes by creating goals. These goals are statements about what your patient wants to change and should be:
- Based on your problem list: The goals should directly relate to substance abuse.
- Broad: Rather than trying to eliminate the behavior, focus on how to introduce positive, healthy behaviors.
- Reasonably achievable: Be sure you and your client agree on goals that they are equipped to complete during the treatment period.
Aim for two to three goals to accomplish while your patient is in substance abuse counseling. Determine what it is they want to accomplish the most and develop the steps they will take to reach that goal. Your treatment will encompass multiple needs of your patient, not just their substance abuse, so their goals may look something like this:
- Developing a healthy relationship with others
- Learning to express negative emotions without using
- Reducing substance intake
- Prioritizing their physical and mental health
- Learning anger management skills
- Improving their quality of life by maintaining abstinence from substances
- Experiencing a difficult life event without using
5. Objectives
While goals and objectives are commonly interchanged terms, they differ slightly when it comes to your counseling notes. Goals are the outcomes of your treatment plan and the things your patient wants to change. Objectives are the concrete, actionable steps you and your patient will take to achieve those goals.
One of the most effective ways to organize your objectives in your counseling notes is to make sure they're SMART:
- Specific: Fits the needs of your patient
- Measurable: Actions that can be observed
- Attainable: Reasonable to achieve
- Relevant: Related to the issues on your problem list
- Time-limited: Have a timeline or target date for completion
6. Interventions
Next, describe the intervention or treatment methods you used or plan to use to complete each of your written objectives. This could be anything from homework you give the client to behavioral experiments. Challenge your patient to take on a new assignment during or after each session to help them address the problems discussed and achieve their treatment goals.
For example, if your client is struggling to control their alcohol use, your intervention may be to monitor their weekly attendance at support group meetings or resolve barriers to attendance, such as childcare services or transportation.
7. Tracking and Evaluating Progress
One of the most important reasons to keep notes as a therapist is to track and evaluate your patient's progress more accurately and effectively. Keeping comprehensive notes and a timeline of how your patient responds to treatment for their substance abuse can help you modify their treatment plan to fit their current needs. You may even write down their:
- Expressed emotions and thoughts
- Behavior
- Demeanor or appearance
- Skills they've learned
- Goals they've achieved
8. Planning Long-Term Care
One of the last steps in completing your notes is to list the next steps for treatment for your patient. In other words, what do you and your patient need to do to achieve the goals and objectives of the treatment plan? During your session, you may discuss long-term care and maintenance options, such as a relapse prevention plan. You may also suggest a support group, a 12-step program, a continuation of therapy long term or prescription medications to assist your patient with substance abuse.
Value of Taking Good Substance Abuse Counseling Notes
Why are good counseling notes so important? With well-written, detailed notes, you can keep your treatment plan organized and monitor your patient's progress more effectively. As a therapist, you likely see tens or dozens of patients regularly.
As you prepare for each appointment, it can be difficult to remember everything you talked about with your patient in the last session, how they're progressing, problems they've recently faced or adjustments you made to their treatment plan. If your notes are illegible, disorganized or not specific enough to remember key details, it can lead to a less productive session and leave both you and your patient feeling frustrated if you have to ask them to repeat themselves.
Common Errors to Avoid
To help make your note-writing process more streamlined, take a look at some common errors that occur when documenting notes and how you can avoid them.
General Statements Without Supporting Data
As a rule of thumb, you should avoid making general statements or including your personal opinions or judgments, especially without any evidence or supporting data that helped you draw those conclusions. If you're writing SOAP notes, for example, your objective section should stick to clearly identifiable facts and specific observations. Without this supporting data, your statements are merely opinions.
Vague Language
Reading through pages of vague notes can make it difficult to follow along and remember key details about your client. If you have to share your notes with other clinicians, you might need to provide more context. Irrelevant information that does not pertain to the client's substance abuse disorder or your session and treatment plan should be left out of your notes.
Likewise, using overly descriptive language can cloud your notes and make your reviewing more time-consuming. When writing any type of therapy note, be straightforward, clear and concise about your client's progress, reactions, statements and needs.
Repetition
Though you may find yourself wanting to restate important details to emphasize major changes or life events for your patient, this will usually make your notes longer, not more effective.
Instead of repeating certain details, compare and contrast progress from previous sessions and determine what adjustments can be made or solutions you can introduce that you have not tried yet. Once you write down your substance abuse counseling notes, try to avoid summarizing them again.
Making Adjustments Instead of Rewriting
As your patient progresses through therapy, you'll likely need to make several changes to their treatment plan and homework exercises. Instead of rewriting your entire treatment plan every time you need to make an adjustment, modify the existing plan where necessary and record the changes you've made so far to the plan along the way. Specify what immediate steps you and your client will take to get closer to the set goals, but don't waste your time rewriting everything when you may only need to make a simple adjustment.
Other common mistakes to avoid include:
- Illegible handwriting
- Failure to sign your notes or include the date and time
- Incomplete or missing documentation
- Adding entries at a later time
- Using incorrect abbreviations
- Writing information in the wrong chart
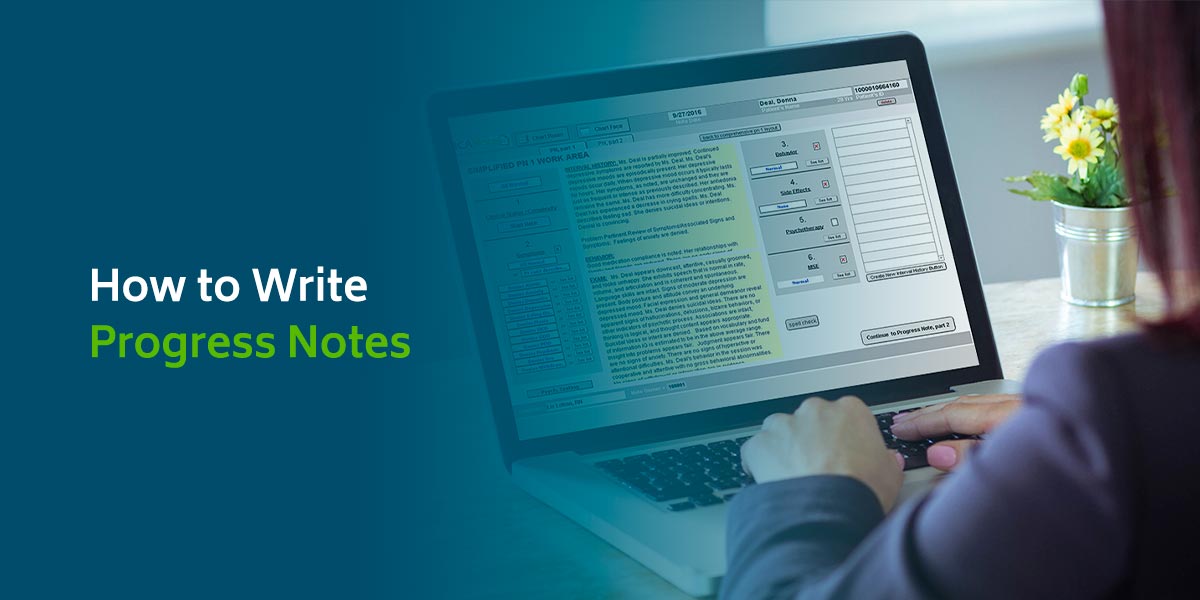
Sample Progress Notes for Substance Abuse Counseling
Let's review how you can use the eight features listed above in your notes to create comprehensive, reliable documentation. Here's a consolidated sample progress note for substance abuse counseling:
- Patient information: Include patient name, diagnosis, medication, mental health history and other relevant details about their substance abuse or session details. You may also include their demographic information, moods, behaviors and symptoms.
- Goals and objectives: Describe the goals and outcomes of treatment and list measurable objectives that will accomplish them.
- Significant concerns or problems: Assess your patient's topics of concern or worry, including patterns of use. These issues will help you monitor and keep track of signs of relapse or distress.
- Interventions: Create specific techniques, methods or exercises your patient can use to achieve their objectives. Begin with small, incremental steps to help increase their confidence in their treatment progress.
- Progress: Develop a personalized way to measure your patient's progress, such as reducing heavy drinking from five times a week to three. Monitoring their outcomes can help you make adjustments for improvement.
6 Tips for Success
Every therapist will have a preference for how they write their notes, but with these six tips, you can make your substance abuse counseling documentation better and more effective:
- Pick a topic for each session: Between you and your patient, decide what you want to focus on for each appointment and try to stick only to that. It can be a certain event, a new concern or other key details your patient has on their mind. By sticking to one topic, you can keep your notes simplified.
- Use a template: Whether you choose to write SOAP notes or the DAP — Data, Assessment, Plan — method, using a template can keep your notes organized and concise. Stick to two to three sentences for each section if possible so you can quickly review your notes when needed.
- Set a timer: To avoid overwriting or taking too long with your notes, setting a timer for 10 or 20 minutes can be helpful. If you cannot finish your notes in that timeframe, assess where you spend the most time on your notes and how you can make them more concise.
- Meet with a colleague or supervisor to do a chart review: If you're not feeling confident in your note-writing abilities, getting feedback from a fellow therapist or supervisor can help you determine where you can improve.
- Remain professional: Because your patient, colleagues or insurance companies may view your notes, remain professional when documenting your observations. Avoid overly negative language, jargon, unique acronyms or anything that sounds like a personal opinion or judgment. Stick to commonly used grammar and terminology so all team members who might read your notes can understand them.
- Introduce EHR software to make note-writing easier: Relying on a robust, intuitive electronic health records (EHR) platform that provides templates for note-writing can make your substance abuse counseling notes more efficient. Whether you need to make notes about symptoms, mental health exams, diagnoses, treatment plans or interventions, you can seamlessly document your notes and keep them organized.
Write Substance Abuse Counseling Notes With ICANotes
No matter what type of therapy counseling notes you write and whether they can be shared with your patient or other colleagues, it’s important to keep them well-organized and streamlined. Spending hours on clinical documentation every day after appointments will cause you to waste valuable time you could be spending with your patients.
At ICANotes, it’s our goal to help behavioral health professionals with all kinds of documentation needs. From complying with HIPAA and Medicare regulations to providing you with templates that make it easier and faster to complete your notes, our clinically robust solution has everything you need to manage your entire workflow. Our note-writing software will help you compile comprehensive notes with less typing and frustration.
To learn more about our solution, contact us today or request a live demo to see how we can help you improve your counseling notes.