How to Address Violent and Aggressive Behavior

Learning about different emotional behaviors and mental health conditions on your path to becoming a therapist certainly makes it easier to help understand and diagnose your patients. However, if your patient is displaying extreme violence or aggression towards you, themselves or others in their life, it's important to know how to effectively address that situation. Some people believe aggression and violence go hand in hand, and while that may be true to an extent, the two behaviors differ in many ways.
As a mental health professional, it's your job to help your patient understand where their aggression and violent behavior comes from and how to manage it. If you've had little to no experience treating people with aggressive or violent behavior, we'll provide some background and tips for how to defuse a hostile interaction with a patient.
Understanding Violence and Aggression
The most important thing to remember about these two behaviors is that while someone who commits violent acts may have aggression, someone with aggression will not necessarily always engage in violence. For instance, a patient throwing an object in a flash of anger during an argument and unintentionally striking their partner is considered aggression, but not necessarily violence. On the other hand, if a patient tells you they shoved their best friend to a wall with the intent of hurting them, that's considered violence.
It's also important to note that aggression can result in both physical or verbal attacks and can be impulsive, defensive or unintentional in nature. Violence may also be impulsive and defensive, but it can also be reactive. Both violence and aggression can result from mental health conditions and environmental factors, and many people express these behaviors in different ways. Sometimes, a single act of violence or aggression can occur as a result of many different triggers or circumstances where your patient feels frustrated, helpless or threatened.
However, it's vital to note that most people who struggle with mental illness are not violent. In individuals with serious mental illness, only about 3% to 5% will become violent. Regardless, it's still important to be aware of the causes of aggression and how it might air out during a therapy session.
Some causes of aggression and violence typically fall into one of these categories:
- Mental health conditions, such as chronic stress, schizophrenia and depression
- Irregular brain development
- Medical conditions like dementia or brain injury
- Side effects from medication
- Hormone imbalances
- Certain genetic mutations
Signs of Possible Aggression or Violent Behavior
As you can see, there are many different reasons why your patient may suddenly display or gradually exhibit aggression and violent behavior. With that in mind, Here are some common signs you may notice with violent patients or aggression that could lead to violence in children, teens and adults:
- Shouting, swearing or making cruel insults or remarks
- Kicking, punching or hitting people or objects
- Bullying or gossiping about someone in their life
- Passive aggressiveness, such as making sarcastic remarks or giving people the silent treatment
- Uncontrollable emotion
- Being overwhelmed by a situation where they were treated unfairly
- Taunting or teasing others to provoke a reaction
- Lying and stealing
- Destroying their own or other people's belongings or property
- Threatening to hurt themselves or others
- Exhibiting impulsive behavior or irritability
- Using manipulation or coercion to maintain control over a person or situation
In addition to these signs, you may also see some direct and obvious hints that your patient is struggling with aggression and violent behavior, such as:
- Having bloodstained hands or clothing
- Pacing or restlessly walking around the room
- Implying or admitting that they have access to a weapon
- Clenching their fists or jaw
- Having hostile facial expressions
- Having difficulty controlling their outbursts or emotions
Types of Aggression and Violent Behavior
As noted above, there are a few different types of aggression and violent behavior, which may characterize how your patient physically or verbally expresses these emotions. Keep in mind that your patient may express their aggression and violence physically, mentally, verbally or emotionally within these categories. Here are the five most common types of aggression that may include violent behavior or that could build up to violent acts:
1. Impulsive Aggression

Sometimes known as affective or emotional aggression, this type of aggression generally stems from the emotions the individual experiences at the moment they commit an aggressive or violent act. With impulsive aggression, your patient may admit to feeling uncontrollable or that their anger came out of nowhere.
The strong emotions associated with impulsive aggression are usually not planned and tend to occur in the heat of the moment. For instance, if your patient gets cut off in traffic and decides to start following them so they can scream and berate them on the road. Or, your teenage patient may impulsively react to a rude classmate by turning off their computer in the library so they lose their work.
2. Instrumental Aggression
Instrumental aggression, also called cognitive or predatory aggression, usually involves some degree of intention and planning that the individual believes will help them achieve a goal. Your patient might exhibit instrumental aggression as a means to an end, whether or not they intend to actually harm someone. This type of calculated aggression generally means that the individual maintains more control over their emotions and is not acting on a whim.
For example, if your patient says that they got too competitive in a friendly game where they knew hurting their opponent would help them win, that's considered instrumental. Or, maybe they've overheard their boss telling their least favorite coworker that they're in line for a promotion that they want, so they decide to spread rumors about their coworker so they can try to obtain the position themselves.
3. Reactive Aggression
Reactive aggression, as the name implies, tends to result as a response to a threat or provocation. With this type of aggression, the individual can become blinded by rage, anxiety or anger and react without a second thought, often causing more harm than intended.
Reactive aggression can be categorized as both a survival tactic and a defensive mechanism, usually characterized by strong emotions and a loss of control. In many cases, a patient may have a justification for reactive aggression, such as the fact that it was their natural instinct to react in such a way.
For example, perhaps your patient accidentally steps on someone's foot at a bar. The person retaliates by shoving them back even though it was an accident, so your patient engages in reactive aggression and ends up in a physical altercation. Or, perhaps your patient found out that their spouse was unfaithful and used reactive aggression by inflicting physical or verbal harm.
4. Expressive Aggression
If your patient is displaying expressive aggression, this means they likely have the intent to exhibit their anger but do not wish to cause harm. However, someone who engages in expressive aggression may feel a sense of satisfaction or even enjoyment from the act, whether that's harming another person, breaking an object or frustrating the person they are targeting with their aggression.
For example, a person who is angry with their spouse and acting with expressive aggression may not thoughtfully intend to cause harm but accidentally damage their spouse's new car when throwing objects around in anger.
Even though the patient did not plan to do that, they may still feel satisfied that they were able to hurt their partner by damaging their new vehicle. Or, maybe they say something cruel to their best friend in the heat of an argument when they didn't intend to, but still get enjoyment out of hurting their friends' feelings.
5. Hostile Aggression
Hostile aggression is perhaps the most concerning and direct of all the types we've discussed. If your patient displays or admits to having hostile aggression tendencies, it generally means they are doing it both on purpose and with the intent to hurt someone. This means they could intentionally plan to harm someone in their lives physically, mentally, verbally or emotionally with the goal of causing them pain.
With children and teens, hostile aggression is often associated with bullying, in which the individual has a fixed mindset to make the other person feel bad. In adults, hostile aggression can often lead to violence and injury, such as starting a physical fight or hitting someone with their car. While all types of aggression must be taken seriously, hostile aggression is particularly alarming and should not be tolerated under any circumstance.
Mental Health Conditions and Violent or Aggressive Behavior
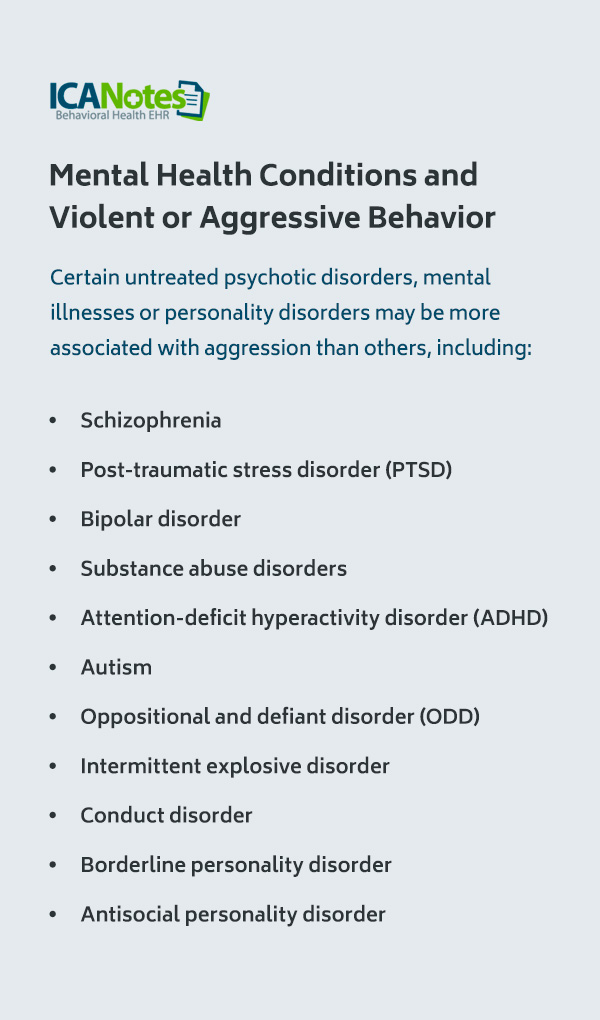
Mental health conditions can sometimes be a contributing factor to excessive aggression or violent behavior. For example, certain untreated psychotic disorders, mental illnesses or personality disorders may be more associated with aggression than others, including:
- Schizophrenia
- Post-traumatic stress disorder (PTSD)
- Bipolar disorder
- Substance abuse disorders
- Attention-deficit hyperactivity disorder (ADHD)
- Autism
- Oppositional and defiant disorder (ODD)
- Intermittent explosive disorder
- Conduct disorder
- Borderline personality disorder
- Antisocial personality disorder
In some cases, mental health conditions may even produce aggressive or violent behavior, such as alcohol and drug abuse, even if an individual is not usually aggressive or violent. Conditions like PTSD can also lead to violent and aggressive thoughts.
Even if an individual does not necessarily have a diagnosed mental health condition, their anger, aggression or violent behavior may occur as a result of growing up in a traumatic environment or suffering neglect, abuse or violence. In fact, children who witness physical violence and other types of abuse are at greater risk of being violent in future relationships.
Traumatic stress can also be a significant factor in heightened aggression. For example, those facing stressful life events and challenges may feel a sense of helplessness and irritability that results in them lashing out, physically or verbally, at their partners and loved ones. Some stressful life changes that can trigger aggression and violence include:
- Divorce or loss of a significant relationship
- Losing a job
- Severe illness or death of a loved one
- Financial difficulty or economic hardship
How Aggression and Violence Impact Mental Health
Just as aggression and violence can come about as a result of mental health conditions, engaging in these behaviors may also make an individual's mental health worse. For instance, if your patient expresses that they had a violent outburst at their place of work, it may have led to disciplinary actions or even termination from their job.
As a result, your patient may struggle to make ends meet financially or become depressed if they are unable to get another job right away, which can all have a negative effect on their mental health. In addition, a person who displays aggression or violent behavior may also struggle to maintain relationships with their long-term partners or loved ones, which can cause them to feel lonely and angrier.
On the flip side, experiencing aggression or violence can also damage a person's mental health and lead to conditions like anxiety, depression or PTSD. Perhaps your patient experienced violence from their recent partner. In this case, they may project their anger and aggression onto others, including their family, friends, coworkers — or therapist.
Regardless of whether your patient displays this aggression and violence in a reactive way as a result of abuse or in an intentional, instrumental way, it's critical to help them understand how it can lead to further mental health issues. If your patient does not have any healthy coping skills to deal with their aggressive and violent tendencies, it may come out in an outburst during your sessions or lead to an altercation between them and their loved ones.
Tips for Treating Violent and Aggressive Behavior: Dos and Don'ts
Now that you have a better understanding of the background of how aggression can lead to violence, it's also important to know how to respond to aggressive behavior. Keep in mind that some individuals who have serious mental illnesses are more prone to aggression and violence while others are not, so it's crucial for providers like yourself to avoid stereotyping certain conditions or making assumptions.
Here are some things you should do during a session with a patient who may become aggressive or violent:
- Redirect the conversation to a topic that does not trigger their aggression.
- Stay calm and be self-aware.
- Keep your voice slow but maintain an assertive tone.
- Encourage them to speak calmly.
- Remain objective.
- Acknowledge the client's feelings.
- Make respectful eye contact.
- Collaborate on a solution.
- Adopt passive body language, such as keeping an open chest.
- Ask open-ended questions to keep them occupied.
- Ensure no other clients are in the area if violence could occur.
- Structure your therapy environment for safety, such as removing any items that could be used as a weapon or installing alarms.
- Position yourself toward the exit.
What to Avoid When Encountering an Aggressive Client
A top strategy for dealing with an aggressive client is to know certain things that you should avoid doing in their presence when a session begins to go south. You should not:
- React to any personal insults they aim at you
- Say anything that could escalate their aggression
- Cross your arms and legs or appear bored with them
- Crowd them or sit too close to them
- Argue with them
- Turn your back to them
- Yell at them, even if they are yelling at you
- Tolerate physical aggression or violence
- Ignore threats of violence — in this case, always exit the room and call for help
- Attempt to disarm a violent person if they have a weapon
Develop Effective Treatment Plans and Notes for Your Patients With ICANotes
As a mental health professional, dealing with an aggressive or violent patient can certainly be stressful at times. Because these behaviors can often result in someone getting hurt or causing your patient to need more intensive therapy, it's critical to keep your therapy notes well-organized and structured so you have a detailed outline of each and every session. With legible, easily accessible notes, you can quickly review your patient's progress and ensure you have all the documentation you need to stay compliant.
With ICANotes, you can access many different therapy templates, tools and document management resources in our intuitive charting solution. Whether you work in an inpatient, outpatient or residential setting, our premier EHR solution has everything you need to speed up documentation time and be more present with your patients who may need your undivided attention. Schedule a live demo or start your free trial to try our features today.