How to Build an Inclusive Mental Health Practice
An inclusive mental health practice is committed to providing accessible, affirming, safe, and equitable mental health care to as many different kinds of clients as possible. This means going out of our way to consider those who have traditionally been excluded from or inadvertently harmed by care due to therapeutic barriers like identity-based discrimination, finances, geography, time, physical space, and rigid therapeutic frames. Below are some things to consider as you build an inclusive therapy practice.
FREE DOWNLOAD: Discover 15 practical strategies to create a more inclusive mental health practice and connect with diverse clients - download this essential guide for mental health clinicians.
Know (and challenge) Your Biases
Since the Black Lives Matter movement surged to the forefront of our collective consciousness in 2020, many in the mental health field committed to implementing Diversity, Equity & Inclusion (DEI) into their practices — particularly providers who hold dominant identities (i.e. cis white women like me). Therapists often describe themselves as inclusive, unbiased, or welcoming everyone regardless of identities - without implementing inclusive practices or understanding what inclusion means in the context of DEI.
There are three letters in DEI for a reason and many people stop at diversity (ensuring representation of people of all races, genders, sexual orientation, ages, body sizes, socioeconomic statuses, abilities, religions). We understand the value of representation and we want everyone to be included. However, without equity and inclusion, diversity alone is guaranteed to be experienced as tokenization and potentially exploitation. Equity is often used interchangeably with “equality” but there is an essential difference: where equality aims to distribute resources evenly, equity aims to thoughtfully distribute resources according to each person’s needs based on the unique barriers they face based on their identities and experiences. Inclusion is only able to exist when diversity exists, when that diverse group has their unique needs met, AND when that group takes the time to become genuinely welcoming and supportive.
In order to build an inclusive mental health practice, we have to build a practice that truly can support a diverse group of people. If your client population is diverse, by definition, you must be wholeheartedly prepared to work with people who are not like you. This requires an honest inventory of your own identities and experiences, as well as an honest inventory of your own limitations and biases. Consider the ways in which you subconsciously assume that your clients think like you, learn like you, feel like you would feel, and have lives like yours. Do some research, hire a DEI mentor, and get comfortable having conversations about privilege and oppression. When working with clients with identities and experiences we do not share, we cannot be fragile, defensive, or avoidant in conversations across differences.
While it’s critical to be non-discriminatory in our practice as therapists, it’s just as important that we are honest with ourselves about our current limitations and biases. In reality, we all have biases, so when we think of (and market ourselves) as “unbiased,” we are significantly more likely to do harm. To deny our biases is a denial of reality — an experience that most clients will find triggering whether they can put their finger on it or not. However, when we have the courage to acknowledge where our biases lie, we have a roadmap for something even better than being unbiased: a lifelong commitment to unlearning and deconstruction. While we don’t have to be (and can never be) unbiased in order to do good therapy, we do have a responsibility to hold, challenge, and — when appropriate — name our biases when they show up in our work with clients. And for those biases which we’ve not yet begun interrogating or we’re in the early stages thereof, I believe it’s more ethical to avoid taking those clients on than to invite people into a room where they are unlikely to experience genuine inclusion.
In this essential webinar, we’ll dive deep into the principles of Diversity, Equity, and Inclusion (DEI) and how they apply to the mental health field. Learn how to challenge your biases, design an equity-informed business model, and implement practical accommodations that foster a safe space for every client. Whether you're new to DEI concepts or looking to enhance your current practices, this webinar will provide valuable tools and strategies to ensure your practice is both inclusive and effective.
What You'll Learn:
➡️ How to recognize and address unconscious biases that may affect your work with clients
➡️ Steps to design an equity-informed business model to ensure fair access to care
➡️ Practical accommodations to improve access to therapy for clients with different identities and abilities
➡️ Adapting therapeutic strategies to meet the unique needs of underrepresented clients
➡️ How to foster a welcoming and safe environment for marginalized groups
Design an Equity-Informed Business Plan
The forever battleground in the private practice therapist’s mind is more than often: money. This work is a personal passion for most of us and we need to be able to pay the bills. We want to help people because we actually care and we literally can’t afford to undervalue our time and expertise to the degree that our bleeding hearts may want us to.
The majority of clients would prefer to access mental health services through their insurance, but on our end, the administrative burdens of paneling and reimbursement are cumbersome at best. A substantial number of therapists opt to forgo insurance altogether, offering superbills for clients to seek reimbursement through out-of-network coverage. While this is a helpful offering, it still limits mental health access to people who have out-of-network benefits (excluding anyone with Medicaid, Medicare, and insurance through the ACA marketplace) and who can afford to front the bill for therapy pending reimbursement. Many therapists also try to compensate for not accepting insurance by reserving a few spots for reduced fee clients, i.e. sliding scale. This is also a fantastic solution, but alone, can lead to revenue loss and ultimately resentment.
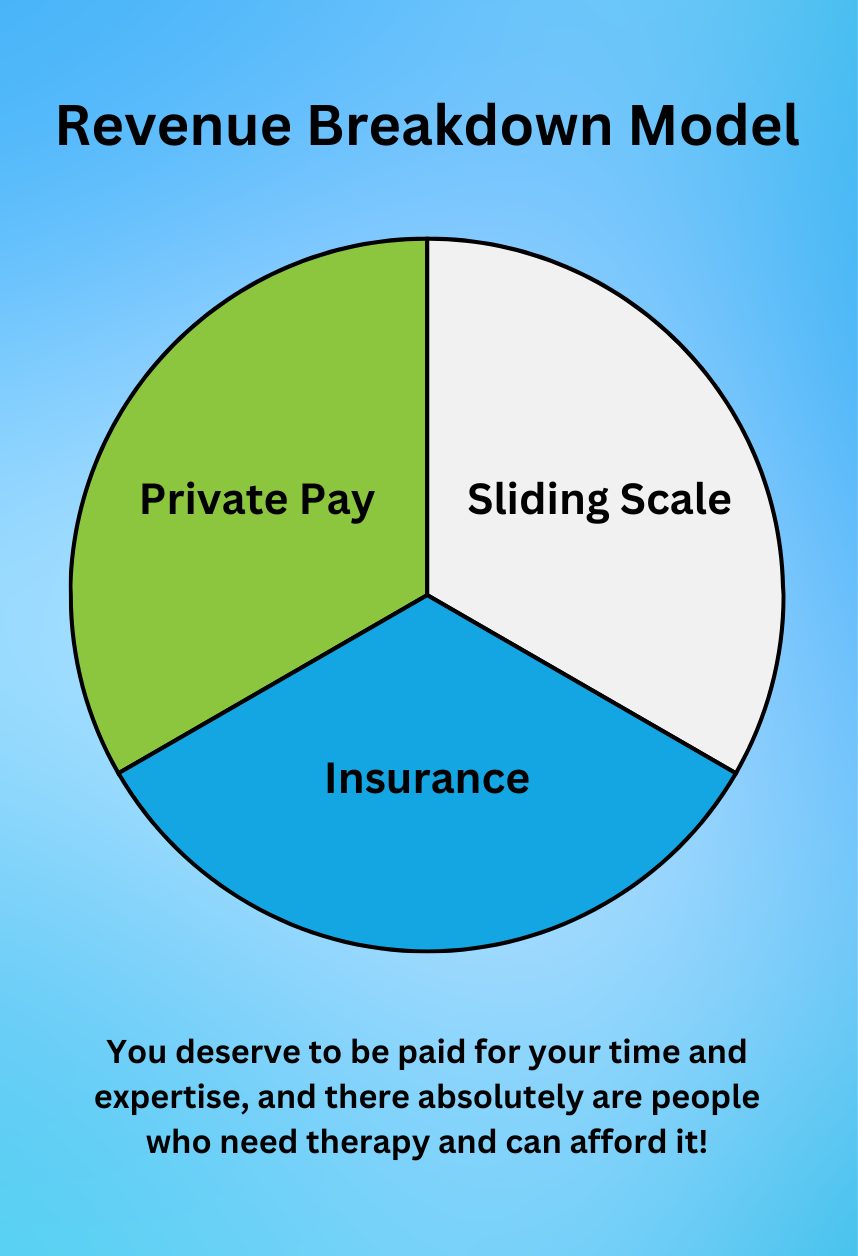
There are many different formats for an equity-informed business plan, but I’ll share mine with you as an example. I have divided my caseload into thirds: one third of my clients pay my full rate out of pocket (superbills offered upon request), one third of my clients are sliding scale (individualized rates based on financial hardship), and one third of my clients use their insurance. I began by determining the number of clients I have time to see in a given week, set my annual revenue goal, and used this as the basis of my math. Then I did some research and selected one insurance company in my state of licensure that I wanted to get paneled with (taking into consideration reimbursement rates and the popularity of the plan). With the likely reimbursement rate of insurance clients in mind, and an estimated average of sliding scale rates, I then calculated my full private pay rate. In loose numbers: if my net annual revenue goal is $140,000 and I have time to see 24 clients (8 of whom use insurance which pays $129/session and 8 of whom are sliding scale at an average of $100/session), then my full fee needs to be $250/session. Whatever your number is, keep in mind that you deserve to be paid for your time and expertise, and there absolutely are people who need therapy and can afford it!
Obviously, you will need to run your own math and consider whatever factors are most relevant for your situation (state of licensure, years of experience, etc), but an equitable model ensures profitability alongside equitable access. The key to making an equitable model work is to actually follow it, limiting the clients you accept to the allocated spots you pre-determined. And while accepting insurance is admittedly a pain, picking just one to get paneled with can both limit the headaches while changing the lives of folks with that insurance who need your care. Whatever structure you design, ensuring that you are able to see clients who cannot afford to pay out of pocket for therapy at full cost is a crucial component of an inclusive therapy practice.
Ensure Access to Your Inclusive Mental Health Services
The pandemic completely changed the mental health field by normalizing telehealth, and one of the benefits of this shift is that folks who face mobility and geographic barriers are now able to seek mental health care despite not being able to physically get to your office. Offering a virtual option for folks who are disabled, have overwhelming work or childcare schedules, live in rural areas, or have transportation limitations is critical. For virtual sessions, it’s important to ensure that you have a HIPAA-compliant option that is accessible via mobile phone for folks who may not have privacy at home or access to a computer.
For neurodivergent folks and/or those who are struggling with executive functioning, it’s important to think through the logistics of your scheduling and payment processes. Some folks might benefit from receiving a calendar invite with the link to the virtual platform for each session. Some folks might need reminders the day before and/or the day of session. Some folks may need to pay with cash for privacy reasons, or need a reminder to pay sent to them after each session. For folks with vision, hearing, or reading comprehension issues, having a website with text-to-voice translation options or a virtual platform with caption options can be a game changer. I often think about how traditional psychotherapy interprets no-shows, late cancellations, and payment lapses as meaningful indicators about the client’s commitment to therapy when many times it may simply have been solved by slight tweaks to process and had no deeper meaning than that they need additional logistical support.
Build in Accommodations
When it comes to seeing clients in-person, it is important to consider the space from the client’s perspective. For gender non-conforming individuals, offering a gender neutral bathroom option can alleviate untold stress from the already emotionally intense experience of being in therapy. For clients of size, it is critical to consider the furniture in the office as well (what is the weight capacity of the furniture? Are there any chairs without arms?). It is also important to know whether your space is ADA compliant and to communicate whether it is in advance of seeing clients in person. Consider also the furniture arrangement — clients with trauma backgrounds often reflect on the importance of sitting somewhere in the room where there is visual contact with the exit. Lastly, many clients benefit from thoughtful details and amenities in the space, including fidgets (helpful for neurodivergent folks), a blanket or pillow (for comfort), snacks (for folks with disordered eating and/or food scarcity), and their own clock to keep track of the time during the session (helpful for folks with anxiety).

Adapt Your Therapeutic Strategies
As we all know, many therapeutic modalities were designed by and for a limited population — usually middle class, white, able-bodied, cisgender people with intact families. These modalities are also often only considering one diagnosis at a time, whereas many folks coming to therapy are navigating a variety of diagnoses at once. For this reason, it’s important to take our clients’ unique situations into consideration when they’re in our care. For example, as an eating disorder therapist, I am aware that Family-Based Therapy (FBT) is widely understood to be the most evidence-based model to use for adolescents with eating disorders. However, some teens with eating disorders are estranged from or have unsupportive family and some don’t have regular access to food, both of which render FBT as-written irrelevant. With some creativity, an inclusive mental health therapist might modify FBT to reimagine what “family” means and incorporate friends or an unrelated but trusted adult instead, or they might look into local food programs and nonprofits that focus on food access to ensure that therapeutic goals can be met.
Whatever therapeutic modalities you utilize, I encourage you to do your research and understand how you might modify your approach to make it workable for people that were not taken into consideration in its development. You can Google whatever the situation you’re navigating looks like, i.e. “DBT with Autism” or “AAPI communities OCD” and see what’s out there. Sometimes there’s a litany of options you didn’t know about and occasionally there’s some new research that’s exploring the same intersections you are. It is highly unlikely that the seemingly niche question you have is being asked for the first time.
Lastly, I want to encourage us all to reconsider the norms and practices we have been trained to hold tightly within our frame. In a typical therapeutic frame, we expect clients make time in their schedule weekly, arrive on time, sit still for 50 minutes, use words to express their emotions, describe their somatic experiences, remember what we discuss, pay us on time, follow through on their intentions between sessions, and lean on their community as needed. While this is also a good summary of my ideal therapeutic frame, there will be clients who cannot participate in therapy this way for reasons outside of their control. Some clients have inconsistent schedules, time blindness, sensory processing issues, verbal processing issues, chronic pain, memory issues, object permanence struggles, and lack of social support for their mental health journey.
As we work towards building an inclusive mental health practice, we are required to step outside of ourselves and imagine the experience through the lens of the people we hope to serve. The onus is on us to create true safety for the clients in our care, and that starts with understanding their needs and building something that works for them. This brings to mind a framework called Universal Design, which posits that when you design something that works for people with the most limitations, it ultimately works better for everyone. When you design a practice that is accessible for someone who is disabled, neurodivergent, fat, nonbinary, BIPOC, and low-income, then you have designed an inclusive mental health practice that is welcoming and supportive to all.
Ready to Create a More Inclusive Mental Health Practice?
Creating an inclusive mental health takes more than just awareness — it requires action. From accessible spaces to supportive tools, every detail makes a difference in your clients' experience. ICANotes equips you with the tools to manage your practice efficiently, so you can focus on offering compassionate, inclusive mental health care to everyone who walks through your door.
Try ICANotes for free and discover how it can help you streamline your practice while fostering inclusivity.
Start your free trial today!

About the Author
Rebecca Eyre, LMHC is a licensed mental health counselor in both New York and Washington state, specializing in eating disorders, trauma, anxiety, and LGBTQ+ issues. She has been practicing since 2011 and is a passionate advocate at the intersection of mental health and social justice. From 2020-2024, she was the CEO of Project HEAL, the leading national nonprofit focused on equitable access to eating disorder care. Rebecca is now in private practice at www.rjetherapy.com.