Is There a Difference Between Telehealth and Telemedicine?
Telehealth and telemedicine are often used interchangeably, and both terms refer to the use of technology to deliver health care remotely. However, there is no standard definition of either of these words, and healthcare organizations use them as they wish. In other words, telehealth terms can get confusing. This post explores the difference between telehealth and telemedicine, what they mean and why virtual health care is on the rise.
The History of Telemedicine
The term telemedicine has various meanings that depend on the organization. According to the World Health Organization (WHO), a study found 104 definitions of telemedicine, which was first coined in the 1970s. WHO describes telemedicine as the "delivery of health care services...by all health care professionals using information and communication technologies." In general, the purpose of telemedicine is to diagnose, treat and prevent disease and injuries.
Although the word telemedicine wasn't used until the 20th century, it traces back to the early 19th century. In 1905, a Dutch physician used telephone wires to transmit electrocardiograms. Then, from the 1920s through the 1940s, physicians provided radio consultations for patients on remote islands or aboard ships. Telemedicine, as we know it today, began in the 1960s in the military and space technology sectors.
Technological advancements and increased availability of communication technology have led to the rapid adoption of telemedicine by health care providers worldwide. Now, all health care providers, from family doctors to mental health counselors, can easily use telemedicine technology to care for clients, whether they live in remote locations or down the street.
The Rise of Telehealth
Telehealth is being commonly used to replace the word telemedicine. The National Institutes of Health defines telehealth as the "use of communications technologies to provide health care from a distance." Telehealth services may be delivered via phone, videoconferencing, text messaging or email. Some doctors use telehealth to monitor patients remotely. For example, a patient might use a device at home to gather vitals or other health data and keep their doctor informed. Countless services may be provided through telehealth, including general exams, mental health counseling and medication consultations.
As telehealth technology continues to improve, and more insurance companies reimburse these services, more health care providers will welcome telehealth in their facilities. The government also plays a role in increasing access to telehealth services. For example, the U.S. Department of Health and Human Services (HHS) encourages health care providers to use telehealth to safely and conveniently treat patients and has taken steps to make it easier to adopt.
The HHS Office for Civil Rights is currently allowing greater flexibility regarding the type of telehealth platforms physicians can use to deliver care. Additionally, the Centers for Medicare and Medicaid Services has greatly expanded its list of covered telehealth services.
Overall, telehealth is becoming widely accepted by health care providers and changing the way patients manage their well-being. It allows health care providers to reach patients in remote or underserved areas, and it's extremely convenient. Currently, many health care providers have adopted telehealth to decrease the spread of illnesses. According to the American Society for Health Care Risk Management, about 15 million Americans received telehealth care in 2016. Now, researchers predict telehealth visits will reach 1 billion by the end of 2020.
Telehealth vs. Telemedicine
As mentioned, telehealth and telemedicine are frequently used interchangeably by health care professionals and various organizations. However, some medical professionals use telemedicine to describe services provided only by physicians and use telehealth as a broader term to signify services delivered by health care providers in general, such as nurses or therapists.
The Office of the National Coordinator for Health Information Technology states that telehealth is not the same as telemedicine because it refers to a wide range of non-clinical services — such as administrative meetings — in addition to clinical services. Telemedicine, on the other hand, relates only to clinical services.
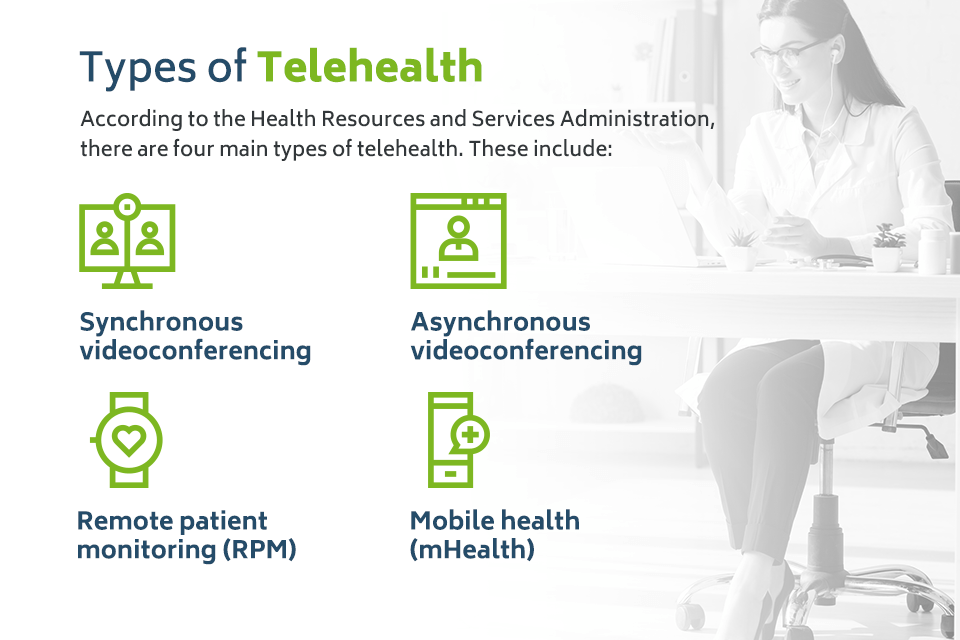
Types of Telehealth
According to the Health Resources and Services Administration, there are four main types of telehealth. These include:
- Synchronous videoconferencing: Synchronous videoconferencing refers to a live, audiovisual link between the clinician and client. With synchronous videoconferencing, the health care provider and patient are present at the same time. For example, a therapist may hold a live therapy session with their client using a telehealth video platform similar to Skype or Zoom but compliant with the Health Insurance Portability and Accountability Act (HIPAA). Telephone calls between the patient and physician are also considered synchronous.
- Asynchronous videoconferencing: Asynchronous videoconferencing, also called store-and-forward, includes the transmission of recorded medical history to a clinician, typically a specialist. A physician might transmit diagnostic images to another doctor electronically to enable a diagnosis. Asynchronous telehealth services may also include emails, secure text messaging or any form of communication that allows both parties to interact at different times. For example, some therapists work for text therapy services and respond to clients within a day rather than immediately.
- Remote patient monitoring (RPM): RPM refers to the use of electronic devices to record medical data, such as vital signs or blood glucose levels, remotely. The data is typically sent to a remote diagnostic testing facility or home health agency for interpretation. RPM may be used to supplement the services of visiting nurses.
- Mobile health (mHealth): MHealth allows patients to monitor and share health information via mobile devices. An example of mHealth includes health tracking apps or wearable devices. MHealth is also used to inform and educate patients about healthcare topics. This may include notifications regarding disease outbreaks or general education information.
Who Uses Telehealth
According to research conducted by the American Medical Association in 2016, only about 15% of physicians used telehealth to interact with patients. Now, nearly half of physicians are seeing patients through telemedicine — up from 18% in 2018. If you've consulted with a client over the phone or communicated with them via email, you've already used telehealth in your practice as well.
Telehealth use is growing across the board and may be used by any health care provider as long as they comply with state and federal laws. This includes:
- Behavioral health professionals: Mental health counselors use telehealth to reach clients regardless of their location and address mental health crises. According to a study from 2018, almost 6 in 10 Americans have sought or have wanted to look for mental health services, either for themselves or a loved one. According to the same survey, 74% of Americans believe mental health services are not highly accessible to the general population. Telehealth provides greater access to mental health care, and it may be a more affordable option for clients.
- General practitioners: General practitioners use telehealth to treat patients in rural areas who otherwise might have to drive dozens of miles to see a doctor. With over 7,200 health professional shortage areas in the country, telehealth allows more patients access to medical services. Family doctors may also meet with patients using a telehealth platform to reduce the number of people in the waiting room and stop the spread of illnesses.
- Speech-language pathologists: As with physicians and behavioral health professionals, telehealth allows speech-language pathologists to reach patients in remote and underserved areas without sacrificing efficacy. According to this review from 2017, studies show that telehealth is a promising method of delivering speech-language services to school-age children.
Other specialists who use telehealth to interact with patients include:
- Physical Therapists
- Radiologists
- Gastroenterologists
- Optometrists
- Occupational Therapists
- Cardiologists
- Obstetricians and gynecologists
- Pharmacists
- Emergency Physicians
- Immunologists
- Dermatologists
- Dentists
Free Ebook: Going Virtual
Everything you need to start a virtual behavioral health practice.
The Pros and Cons of Telehealth
Telehealth continues to grow because it offers many advantages for clinicians and their patients. Here are some reasons to consider providing telehealth as a behavioral health professional:
- Offer convenience: Telehealth is convenient for the patient and practitioner. With telehealth, patients receive medical or mental health care without needing to leave their homes. They don't have to worry about driving, dealing with traffic or finding a ride if they don't have a car. They also don't have to waste time sitting in a waiting room before appointments. Likewise, clinicians may also work from their chosen location and may not have to deal with a commute.
- Enable flexibility: Telehealth allows clinicians to work outside of regular office hours. Therefore, they can enjoy a better work-life balance and offer services at times that better suit their patients.
- Be effective: In many cases, telehealth is just as effective as in-person services. For example, a review from 2017 looked at various research articles to determine whether telehealth is an effective alternative for mental health services. Researchers concluded that telehealth is just as effective as in-person services when caring for patients with mental illnesses. It offers many advantages, such as reaching isolated communities and providing more affordable care for patients.
- Increase patient satisfaction: Many patients appreciate the convenience of telehealth and find the services just as satisfactory as in-person appointments. For example, according to a study conducted at Massachusetts General Hospital, 79% of patients found virtual visits convenient, and 62% said the visit was of the same quality as an in-person appointment. Mental health services, in particular, are well-suited for telehealth.
- Stay safe: Since you will not see clients in person when you provide telehealth services, you do not have to worry about infection control. This also allows you to work confidently with clients who are at high risk of developing complications resulting from an infection. You and your clients can also avoid weather-related hazards like icy roads because you won't have to drive anywhere to deliver services.
- Reduce expenses: Even if you decide to offer both telehealth services and in-person sessions, you can still save on costs such as utilities and office supplies, because you won't need to use your office as much.
- Simplify communication: If you use an electronic health record (EHR) system with a telehealth feature, such as ICANotes, you can communicate with patients more easily and help them manage their appointments. For example, with ICANotes, you can send automatic appointment reminders via text or email and remove the need to call clients.
- Enjoy a comfortable setting: Telehealth allows you to work from home. That means you can make your environment as comfortable as you wish, and you'll always have access to your own food and bathroom. During breaks, you can fit in a quick workout or take your dog for a walk. Overall, you can improve your well-being when you work from home, and give your best self to your clients.
- Improve access to care: With telehealth, you're not limited by space or time. You can serve clients who live in remote communities, are incarcerated or can't leave their homes due to a physical disability. By accepting more patients, you can grow your practice and help your region at the same time.
- Enhance privacy: Almost a third of Americans have worried they'll be judged by others if they receive mental health services. Since telehealth allows clients to stay at home, they can obtain services in private and avoid worrying about being seen by neighbors or other clients.
If you're considering starting a virtual practice, you'll also want to think about some of the challenges you might face. Here are a few disadvantages:
- May not be covered: Although most insurance companies offer some sort of telehealth coverage, some insurers may not provide benefits for virtual care.
- Could experience technological issues: Health care providers may experience technical difficulties when providing telehealth services, either on their or the patient's end. For example, a patient may not have the right internet speed to produce a quality video, or they may get disconnected due to a power outage. You'll need to have a backup plan to get through technical issues.
- May require an in-person visit: Depending on the situation, a patient may need to come into the office to receive a proper diagnosis. For example, they may not be able to take their own vital signs if they don't have the right instruments. Also, if the lighting is poor, a doctor can't see a client's complexion. Nor can they assess their ears, nose and throat. A physician must consider if telehealth is right for the patient, depending on their symptoms or medical history.
- Does not suit all patients: Although telehealth is an excellent choice to help patients with depression or anxiety, it may not be the best option for clients in need of intensive care.
- Can raise privacy concerns: As a health care provider, you need to ensure you use telehealth software that complies with privacy laws. Patients should also keep their confidentiality in mind and avoid attending telehealth appointments in public places.
Telemedicine, Telehealth, and Telepractice?
You may have come across the term telepractice, which is not the same as telemedicine or telehealth. The American Speech-Language-Hearing Association defines telepractice as the use of communications technology to deliver speech-language pathology and audiology services remotely. Telepractice is used instead of telemedicine or telehealth to prevent patients from thinking that virtual services are only used in medical settings.
As a behavioral health professional, you might use other terms to describe telehealth services as well, such as online therapy, teletherapy or telemental health.
Try Telehealth With ICANotes
If you're ready to offer your clients telehealth services, now is the ideal time to start. The ICANotes EHR for behavioral health can help you seamlessly transition into a virtual practice. With the ICANotes integrated telehealth feature, you'll enjoy an easy-to-use, HIPAA-compliant videoconferencing platform that launches directly from your EHR interface. To experience ICANotes and see how it works, please sign up for your free trial.
Sources
- https://mhealthintelligence.com/features/is-there-a-difference-between-telemedicine-and-telehealth
- https://www.ashrm.org/sites/default/files/ashrm/TELEMEDICINE-WHITE-PAPER.pdf
- https://www.who.int/goe/publications/goe_telemedicine_2010.pdf
- https://medlineplus.gov/telehealth.html
- https://telehealth.hhs.gov/patients/understanding-telehealth/
- https://www.healthit.gov/topic/health-it-initiatives/telemedicine-and-telehealth
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3089841/
- https://www.healthcareitnews.com/news/patient-experience-evolving-providers-embrace-telehealth
- https://www.hhs.gov/coronavirus/telehealth/index.html
- https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html
- https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes
- https://go.forrester.com/press-newsroom/us-virtual-care-visits-to-soar-to-more-than-1-billion/
- https://www.healthit.gov/faq/what-telehealth-how-telehealth-different-telemedicine
- https://www.healthline.com/health/mental-health/text-therapy#cost
- https://www.imedicalapps.com/2012/05/synchronous-asynchronous-communication/
- https://www.americantelemed.org/resource/why-telemedicine/
- https://www.businessinsider.com/mhealth-apps-definition-examples
- https://www.merritthawkins.com/uploadedFiles/Corona_Physician_Survey_Merritt_Hawkins_Report.pdf
- https://www.ama-assn.org/practice-management/digital/which-medical-specialties-use-telemedicine-most
- https://www.medicaid.gov/medicaid/benefits/downloads/medicaid-chip-telehealth-toolkit.pdf
- https://medlineplus.gov/ency/patientinstructions/000919.htm
- https://www.aamc.org/news-insights/attracting-next-generation-physicians-rural-medicine
- https://otpotential.com/blog/telehealth-occupational-therapy
- https://www.cohenveteransnetwork.org/wp-content/uploads/2018/10/CVN_Infographic_10.8.18_1045am.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5546562/
- https://www.hopkinsmedicine.org/telemedicine/about.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5723163/
- https://ibcces.org/blog/2020/06/09/reasons-teletherapy-benefits-a-speech-language-pathologist/
- https://www.massgeneral.org/news/press-release/virtual-video-visits-may-improve-patient-convenience-without-sacrificing-quality-of-care-communication
- https://www.fshealth.com/blog/29-statistics-about-telemedicine-healthcare
- https://www.medicalnewstoday.com/articles/telemedicine-benefits#summary
- https://health.usnews.com/health-news/articles/2012/07/24/pros-and-cons-of-telemedicine-for-todays-workers
- https://www.asha.org/Practice-Portal/Professional-Issues/Telepractice/